Drug-coated balloon catheters to open narrowed blood vessels and to deliver drugs to the impacted sites are used frequently for the treatment of peripheral arterial disease. Scientists believe improvement of the coatings could lead to better designs and improved outcomes. Now for the first time, researchers at Boston University School of Medicine (BUSM) have examined these coatings at microscopic levels in hopes of producing more efficient alternatives for treating arterial disease.
Obstructive arterial disease is a clinical challenge affecting millions of people in the world. Devices such as stents and balloon catheters are the primary choice for treating these narrowed vessels. While the use of stents is beneficial in many cases, once implanted, they remain in the body permanently. Presence of such foreign bodies inside an artery can lead to unexpected complications in some patients. Therefore, using a drug-coated balloon to open the narrowed vessel and immediately deliver medications to the site is an attractive strategy because there is no device left within the vessel after the procedure.
“Unfortunately, the delivery of drugs within a short period of time is extremely inefficient (less than 10 percent). It is important to understand how to improve delivery efficiency and also understand the mechanisms driving acute drug transfer and coating adhesion to the artery,” explained corresponding author Vijaya B. Kolachalama, Ph.D., assistant professor of medicine at BUSM.
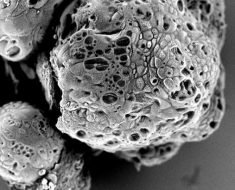
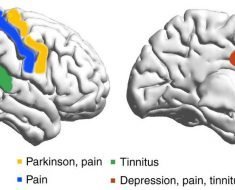
The researchers performed a series of experiments including compression testing to measure the mechanics, scanning electron microscopy to examine the intrinsic coating structure and cell cultures to quantify drug toxicity. They also developed a biophysical model to illustrate the interactions between the balloon coating and the artery during balloon angioplasty.
They found that microscopic particles of some coatings have needle-like shapes and some have spherical shapes and that these shapes determine the mechanics of contact between coating and the artery, which in turn influences the amount of drug transfer to artery. “Ultimately, this affects the device performance and the outcomes.”
Source: Read Full Article