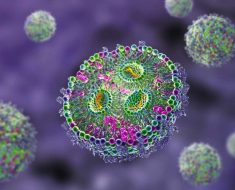
A simple to use, paper-based test for the novel coronavirus in wastewater could help identify the infection in communities, including those with people who carry the virus but show no symptoms.

In January 2020, doctors treating the first confirmed case of COVID-19 in the United States identified the SARS-CoV-2 virus not only in nasal and oral swabs but also in stool samples.
This has led scientists in the U.K. and China to propose that wastewater in sewer systems could provide early indications of the spread of the virus among communities.
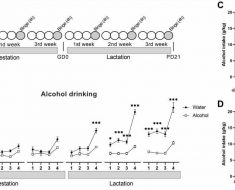
Wastewater-based epidemiology is already widely used in the U.S. and Europe to gauge the extent of illicit drug use.
Stay informed with live updates on the current COVID-19 outbreak and visit our coronavirus hub for more advice on prevention and treatment.
It can also provide data about dietary factors, such as sugar intake and alcohol consumption, as well as exposure to environmental toxins.
Zhugen Yang, Ph.D., a lecturer in sensor technology at Cranfield University’s Water Science Institute, in the U.K., and a team of scientists at the Chinese Academy of Sciences, in Guiyang, describe the proposed test in the journal Environmental Science & Technology.
It is possible for people carrying the new coronavirus to experience few or no symptoms. In this case, doctors consider them to be “asymptomatic.” The team of researchers explain that this circumstance can be dangerous:
“Without the ability to screen these asymptomatic patients quickly and effectively, these unsuspecting carriers have the potential to increase the risk of disease transmission if no early effective quarantine measures are implemented.”
Earlier, working with colleagues at the University of Glasgow, in the U.K., and Uganda’s Ministry of Health, Yang developed a paper-based test for malaria using the same technology.
The device, which costs less than 50 cents, uses a sample of blood and can distinguish between types of malaria infection. This is especially beneficial in rural communities that are far from specialized laboratories. The team described the test in the journal PNAS in 2019.
Range of targets
Currently, paper-based devices can detect a range of other pathogens as well, including the Zika virus, Salmonella, and HIV.
Yang believes that the technology, which gives rapid, on-the-spot results, could be adapted to detect SARS-CoV-2 in wastewater.
“If COVID-19 can be monitored in a community at an early stage through [wastewater-based epidemiology], effective intervention can be taken as early as possible to restrict the movements of that local population, working to minimize the pathogen spread and threat to public health.”
– Zhugen Yang, Ph.D.
Existing tests for pathogens such as SARS-CoV-2 must be performed by skilled technicians using elaborate equipment in laboratory settings. The tests can take up to 6 hours to deliver results.
By contrast, a paper-based test could be carried out in situ by nonspecialists without any cumbersome equipment or power source. It could give a result in around 50 minutes.
The paper device developed by Yang for malaria is designed to be folded repeatedly in a specific pattern, as in origami.
Each fold brings the sample into contact with a series of filters and reagents embedded in the device. These isolate tiny amounts of genetic material in the sample, amplify them, and detect the presence of DNA or RNA sequences in particular pathogens.
A green circle indicates a positive result and a red circle a negative result.
Safe disposal
Paper analytical devices are compact and lightweight, making them easy to store and transport. They can be incinerated after use to prevent contamination.
When Medical News Today contacted Yang, he emphasized that it could take up to 1 year to fully develop and validate a device for detecting the novel coronavirus.
Further development of the test is being sponsored in the U.K. by the Natural Environment Research Council and the Royal Academy of Engineering.
For live updates on the latest developments regarding the novel coronavirus and COVID-19, click here.
Source: Read Full Article