Severe fatty liver disease is commonly associated with obesity, but according to a review of scientific literature conducted by researchers at Temple University and the Translational Genomics Research Institute (TGen), an affiliate of City of Hope, there is a growing body of evidence suggesting that even normal weight individuals can contract this potentially life-threatening condition.
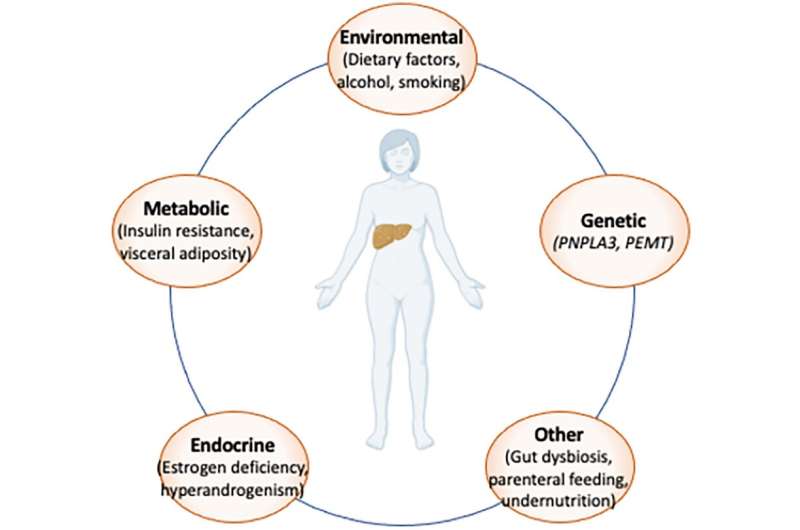
Why this occurs is poorly understood, though some of the suspected liver-disease risk-factors for lean individuals include diet, genetics, ethnicity, and even menopausal status for women, according to the scientific review published today in the journal Diabetology and Metabolic Syndrome.
“Because fatty liver disease, in most cases, is a clinically silent condition, the absence of early signs and symptoms, coupled with normal laboratory and body measurements, blind clinicians to the presence of severe liver disease in normal weight individuals,” said Johanna DiStefano, Ph.D., Professor in TGen’s Metabolic and Fibrotic Disease Program, and head of TGen’s Diabetes and Fibrotic Disease Unit.
Nonalcoholic fatty liver disease (NAFLD) is the most common chronic liver condition in the U.S., and may affect an estimated 24% of the global population. The incidence of NAFLD is climbing worldwide, making it a significant health threat. Its most severe form can progress to a condition called nonalcoholic steatohepatitis (NASH), which is characterized by liver inflammation and oftentimes fibrosis, and can lead to cirrhosis, cancer of the liver, and death. All are difficult to diagnose and treat.
Surprise finding for lean patients
One study showed that between the time they were initially diagnosed and follow-up examinations, lean individuals with NAFLD were at greater risk for developing severe liver disease than those with higher body mass index (BMI).
“This unexpected finding suggests that lean individuals experience a faster rate of fibrosis progression compared to those with higher BMI,” Dr. DiStefano said.
While obesity is the strongest independent risk factor for NAFLD, even in cases of severe obesity some individuals do not develop severe liver disease, suggesting there may be genetic factors at work; some genes that promote liver disease, and others that are protective against the condition.
For example, one study of more than 900 lean Japanese participants showed a doubling of NAFLD risk among those who carried the well-studied PNPLA3 gene.
Also, women are at high risk of developing NAFLD following the menopausal transition, likely due to hormone-related metabolic changes resulting from the loss of protective estrogens and other factors, the review said.
No consensus on NAFLD screening
There is no global consensus for how to screen for NAFLD due to the uncertain evidence supporting diagnostic tests, treatment options, cost-effectiveness and the potential long-term benefits of screening. And for lean individuals, guidelines for NAFLD are even less clear:
“The development and distribution of consistent screening and risk assessment guidelines will be critical to ensure optimal clinical management for all NAFLD patients,” the review said.
Assessing NAFLD risk among lean individuals may depend on greater awareness of menopausal status, genetic factors, ethnicity—especially among those of Asian Indian and Hispanic ancestry—alcohol consumption, and dietary factors, including added sugars, refined carbohydrates, saturated fat and cholesterol. A major question is whether NAFLD in lean individuals represents a distinct disease requiring specific management, as suggested by many researchers, or is it a type of classical obesity-associated NAFLD that will respond to the current approach of weight loss, and the control of insulin resistance, high blood pressure, and excessive fat in blood?
“Much more work is needed not only to address risk factors but also to promote greater awareness among practitioners about the potential health risks associated with NAFLD among lean individuals,” said Glenn S. Gerhard, M.D., Chair of the Department of Medical Genetics and Molecular Biochemistry at the Lewis Katz School of Medicine at Temple University.
Source: Read Full Article





