In a recent study published in the journal Cell, researchers explored neurological symptoms and subsequent cognitive impairment experienced by survivors of mild respiratory coronavirus disease 2019 (COVID-19).
Study: Mild respiratory COVID can cause multi-lineage neural cell and myelin dysregulation
Background
Studies have shown that approximately one in four COVID-19 survivors experience neurological symptoms with persistent cognitive impairment. An impaired memory, attention, concentration, and reduced speed of information processing characterizes this syndrome, commonly referred to as brain fog.
The COVID-19-associated cognitive impairment with increased anxiety, depression, disturbed sleep, and fatigue contributes substantially to the development of long COVID, thus representing a major public health crisis. In many cases, people face difficulties in attaining full occupational function. This syndrome resembles cancer therapy-related cognitive impairment, colloquially known as chemo-fog. The patients of both these syndromes experience neuroinflammation and white matter-selective microglial reactivity.
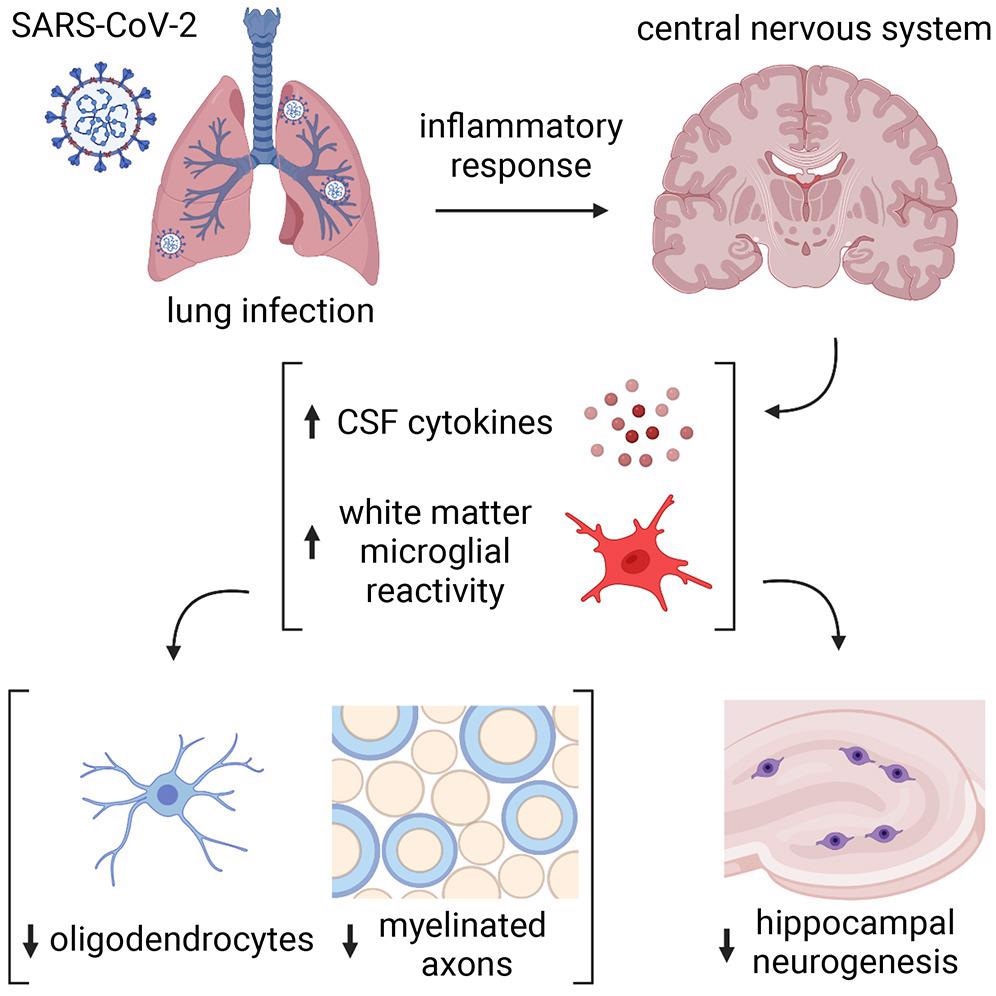
Microglial reactivity impairs mechanisms of myelin-forming oligodendrocytes and the synthesis of new neurons in the hippocampus. Other effects include elevated cerebrospinal fluid (CSF) cytokines or chemokines, including C-C motif chemokine 11 (CCL11).
About the study
In the present study, researchers used a mouse model to test the effects of mild respiratory COVID-19. First, they delivered human angiotensin-converting enzyme 2 (hACE2) receptor via an adeno-associated virus (AAV) vector to the trachea and lungs of test animals. Two weeks later, they intranasally delivered severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) into these mice.
The team also investigated human cortex and subcortical white matter samples from nine individuals who were SARS-CoV-2 positive between March and July 2020. Further, the researchers compared the chemokine and altered homeostatic gene signatures to pathology-specific reactive microglial states, including disease-associated microglia (DAM) observed in Alzheimer's and white matter-associated microglia (WAM) observed in aging.
Study findings
The mild respiratory COVID-19 in the test animals resulted in prolonged changes in cytokines within the central nervous system (CNS). Accordingly, the authors observed elevated CCL11 levels in the serum of mice at seven days post-infection (pi). In contrast, CCL11 levels in CSF normalized by seven weeks pi. Notably, the authors did not observe any weight loss, observable sickness behavior, and viral presence in the brain of infected mice.
Further, the authors observed increased microglial reactivity in the subcortical white matter of two mouse strains, CD1 and BALB/c, at seven days pi, which persisted till seven weeks. Conversely, there was no microglial reactivity in the cortical gray matter; however, overall numbers of microglia remained unchanged. Like the test mice, humans with COVID-19 exhibited elevated microglial reactivity in subcortical white matter.
The single-cell ribonucleic acid (RNA) sequencing of cortical and white matter microglia seven days following mild respiratory COVID-19 revealed five distinct microglial states. Compared to the control mice, mildly infected mice had an increased abundance of the chemokine-enriched microglia and profound transcriptional changes within the homeostatic microglia cluster. Accordingly, the homeostatic microglia cluster showed downregulation of three genes, as follows:
i) triggering receptors expressed on myeloid cells 2 (TREM2),
ii) spalt-like transcription factor 3 (SALL3), and
iii) adrenoceptor beta 1 (ADRB1) genes
Gene ontology (GO) highlighted the upregulation of cytokine production, cytotoxicity, and immune responses. The finding indicated that although not 'fully' reactive microglia had an altered function following SARS-CoV-2 infection. In addition, the altered homeostatic gene signatures in post-COVID-19 microglia showed the highest similarity to the WAM and DAM states. However, none of these states completely encompassed the respiratory COVID-19-related transcriptional changes, indicating a distinct microglial reactivity state following mild respiratory COVID-19.
The electron microscopy ultrastructural analyses also revealed loss of myelin, the insulating ensheath of axons that provide metabolic support to axons. This decrease was evident at seven days pi by SARS-CoV-2 and persisted till seven weeks and was similar in magnitude to the loss of myelinated axons after four weeks to six months of methotrexate chemotherapy.
Conclusions
The current study demonstrated that even mild SARS-CoV-2 infection could cause neurological changes that may dysregulate neural cells crucial for healthy cognitive functions. Contrastingly, H1N1 influenza elicited a more restricted pattern of persistent neural cell changes, i.e., only elevated CCL11 levels and hippocampal pathology. Furthermore, the oligodendroglial deficits observed in the study resembled more with the changes that followed methotrexate chemotherapy. Future studies should further elucidate the mechanisms mediating respiratory infection-induced subcortical white matter microglial reactivity, also involving cytokine signaling mechanisms or cellular neural-immune interactions.
- Mild respiratory COVID can cause multi-lineage neural cell and myelin dysregulation, Anthony Fernández-Castañeda, Peiwen Lu, Anna C. Geraghty, Eric Song, Myoung-Hwa Lee, Jamie Wood, Michael R. O'Dea, Selena Dutton, Kiarash Shamardani, Kamsi Nwangwu, Rebecca Mancusi, Belgin Yalçın, Kathryn R. Taylor, Lehi Acosta-Alvarez, Karen Malacon, Michael B. Keough, Lijun Ni, Pamelyn J. Woo, Daniel Contreras-Esquivel, Angus Martin Shaw Toland, Jeff R. Gehlhausen, Jon Klein, Takehiro Takahashi, Julio Silva, Benjamin Israelow, Carolina Lucas, Tianyang Mao, Mario A. Peña-Hernández, Alexandra Tabachnikova, Robert J. Homer, Laura Tabacof, Jenna Tosto-Mancuso, Erica Breyman, Amy Kontorovich, Dayna McCarthy, Martha Quezado, Hannes Vogel, Marco M. Hefti, Daniel P. Perl, Shane Liddelow, Rebecca Folkerth, David Putrino, Avindra Nath, Akiko Iwasaki, Michelle Monje, Cell 2022, DOI: https://doi.org/10.1016/j.cell.2022.06.008, https://www.cell.com/cell/fulltext/S0092-8674(22)00713-9
Posted in: Men's Health News | Medical Research News | Medical Condition News | Women's Health News | Disease/Infection News
Tags: Aging, Angiotensin, Angiotensin-Converting Enzyme 2, Anxiety, Brain, Brain Fog, Cancer, Cancer Therapy, CCL11, Cell, Central Nervous System, Chemokine, Chemokines, Chemotherapy, Coronavirus, Coronavirus Disease COVID-19, Cortex, covid-19, Cytokine, Cytokines, Cytotoxicity, Depression, Electron, Electron Microscopy, Enzyme, Fatigue, Gene, Genes, H1N1, Hippocampus, Influenza, Lungs, Methotrexate, Microglia, Microscopy, Mouse Model, Myelin, Nervous System, Neurons, Pathology, Public Health, Receptor, Respiratory, Ribonucleic Acid, RNA, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Sleep, Syndrome, Transcription, Virus, Weight Loss

Written by
Neha Mathur
Neha is a digital marketing professional based in Gurugram, India. She has a Master’s degree from the University of Rajasthan with a specialization in Biotechnology in 2008. She has experience in pre-clinical research as part of her research project in The Department of Toxicology at the prestigious Central Drug Research Institute (CDRI), Lucknow, India. She also holds a certification in C++ programming.
Source: Read Full Article