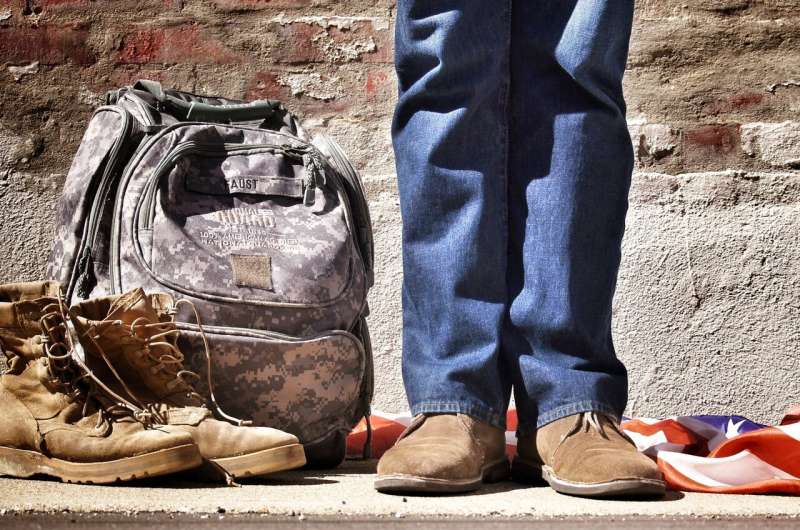
A study of post-9/11 veterans shows that those with moderate or severe traumatic brain injury (TBI) who have never been deployed have a higher risk of epilepsy than those who have been deployed. The study is published in Neurology.
“We anticipated that deployment would be linked to a higher risk of epilepsy among post-9/11 veterans with TBI given the potential higher risk for a blast or combat exposure,” said study author Mary Jo V. Pugh, Ph.D., RN, of VA Salt Lake City in Utah and a Fellow of the American Academy of Neurology.
“However, we found that epilepsy was more common among those with moderate TBI who had never been deployed. This may be explained by the ‘healthy warrior effect,’ where good health is required for deployment. We found those who had not been deployed had higher percentages of epilepsy risk factors, including brain tumors, stroke, and other neurologic diseases.”
TBI is caused by a bump, blow or jolt to the head or by an injury to the head caused by falls, motor vehicle crashes or assaults. With moderate TBI a person loses consciousness for up to a day. Severe TBI involves losing consciousness for more than a day.
Pugh said the study also found that among those who had penetrating TBI, the most severe type of TBI, the risk of epilepsy was higher for deployed vets. Penetrating TBI can be caused by bullets, shrapnel, knives or other sharp objects.
The study involved 938,890 post-9/11 veterans with an average age of 35. Of the total participants, 71% had been deployed and 2.9% had epilepsy. Epilepsy was more common among veterans who were never deployed with 3.9% versus those who were deployed with 2.5%.
Researchers looked at medical records to determine which participants had TBI and what level of TBI. Overall, 14% of non-deployed veterans had TBI and 34% of deployed veterans had TBI.
When looking at TBI severity, researchers found that epilepsy risk for those with mild TBI did not differ by deployment status, but there were differences by deployment status for those with more severe TBI.
Researchers found that 1.2% of non-deployed veterans and 2.5% of deployed veterans had moderate or severe TBI. After adjusting for age, sex, and other risk factors for epilepsy, they found that among those with moderate and severe TBI, those who were not deployed were nearly three times more likely to have epilepsy and those who were deployed were two times more likely to have epilepsy when compared to those without TBI.
They also found 0.2% of non-deployed veterans and 0.5% of deployed veterans had penetrating TBI. Of the veterans who had penetrating TBI, those who were not deployed were four times more likely to have epilepsy, and those who were deployed were more than five times more likely to have epilepsy when compared to those who did not have TBI.
“Closer monitoring for epilepsy among those with more risk factors for the disease may help shorten the time to diagnosis and appropriate treatment,” Pugh added.
A limitation of the study is that results may not be generalizable to other veteran groups, such as older veterans, due to their differing war exposures.
More information:
Neurology (2023).
Journal information:
Neurology
Source: Read Full Article