Americans’ use of common outpatient health services dipped sharply at the outset of the COVID-19 pandemic, then rebounded to near-normal levels by the end of 2020, only to decline again during the second surge in January–February 2021, according to a new UCLA-led study.
But the 2020 recovery in care wasn’t equal for all, researchers found. Some of the most socioeconomically disadvantaged patients—those with Medicaid or Medicare-Medicaid dual eligibility insurance—were far less likely than those with other insurance plans to return to using outpatient services at rates approaching normal, pre-pandemic levels.
The study, published this week in the Journal of the American Medical Association and based on data on 14.5 million adults in the U.S., raises concerns about patients missing treatments for acute illnesses, delaying preventive care and lacking a clear understanding of when to seek help during the pandemic, said lead author Dr. John Mafi, an associate professor of medicine and practicing general internist at the David Geffen School of Medicine at UCLA.
“The worsening access to care we observed among socioeconomically disadvantaged Americans is particularly concerning,” Mafi said, “because it suggests that the pandemic is widening inequities in access to vital health services such as emergency care, preventive cancer screening and behavioral health services.”
For the study, the researchers looked at the use of six ambulatory care services: emergency department visits, doctors office visits (including for urgent care), behavioral health services, colonoscopy screenings, mammogram screenings, and HIV screenings or contraception counseling. They compared the utilization of those services among patients with commercial insurance, Medicare Advantage, Medicare fee-for-service insurance, and those with Medicaid or Medicare-Medicaid dual eligibility insurance between Jan. 1, 2019, and Feb. 28, 2021. (Patient data was drawn from the Milliman MedInsight Emerging Experience research database and included data on patients from all U.S. states.)
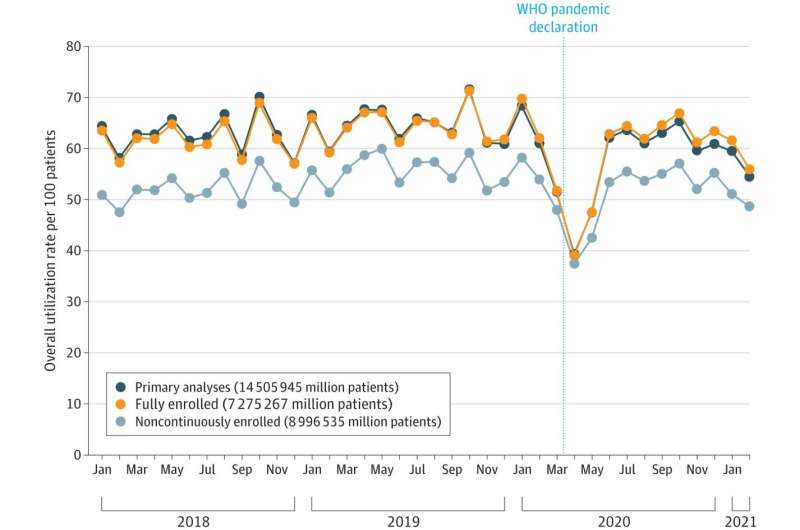
They found that during the initial COVID-19 surge in March–April 2020, overall use of the six ambulatory care services dropped to just 67 percent of levels that would be expected had the pandemic not occurred.
In those early months of the pandemic, the Centers for Medicare and Medicaid Services instructed hospitals and medical practices across the nation to curb some outpatient services to preserve resources for more critical care and to minimize COVID-19 transmission, the researchers noted. In addition, many patients canceled scheduled outpatient appointments out of fear of contracting the virus. As a result, many people did not receive outpatient care they otherwise would have.
However, by November–December 2020, utilization of the six outpatient services rebounded to 97 percent of expected rates. During the second surge, in January–February 2021, overall utilization dropped again, to 86 percent of expected rates, and the return to expected rates varied by insurance type, with Medicaid and Medicare-Medicaid dual eligible patients having lower rates of recovery:
- Commercial insurance: 91 percent
- Medicare Advantage: 83 percent
- Medicare fee-for-service: 81 percent
- Medicaid: 78 percent
- Medicare-Medicaid dual eligible: 73 percent
The study authors said there remains a need to understand the reasons for persistently delayed care, particularly among socioeconomically disadvantaged patients, and to consider various approaches to addressing this challenge.
“Policymakers, health system leaders, clinicians and patients should proactively develop rapid and effective ‘catch-up’ strategies to avoid harm that could result from missed opportunities for care during the pandemic,” said senior author Dr. Katherine Kahn, a distinguished professor of medicine and practicing general internist at the Geffen School. “Patients at high risk for adverse health outcomes associated with missed care during the pandemic or during the period leading up to it may need additional efforts to overcome barriers to accessing ambulatory care.”
Kahn emphasized that ongoing efforts to educate patients about timely symptom-based and preventive care, paired with expanded telemedicine outreach and community engagement programs—in the context of commitments to equity, diversity and inclusion—could make a big difference.
Source: Read Full Article