- In a recent study, researchers investigated whether it’s possible to predict cognitive decline based on the presence of amyloid and tau proteins in the brain.
- They found that the presence of both amyloid and tau proteins in the brain of cognitively healthy individuals is linked to short-term cognitive decline.
- The researchers hope that amyloid and tau PET brain scans may be used to identify individuals at risk of cognitive decline, allowing them to receive earlier interventions.
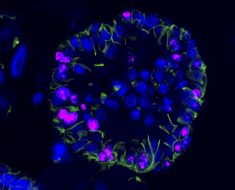
Alzheimer’s disease (AD) is characterized by memory loss, language problems, impulsive or unpredictable behavior, and elevated levels of beta-amyloid and tau proteins in the brain, which form distinctive plaques and neurofibrillary tangles.
Currently, about 1 in 9 people ages 65 and older (10.7%) have AD. More than 6 million Americans are estimated to have AD, and the number is expected to double by 2050.
Given the social and economic burden of AD, great research efforts have been dedicated to diagnosing and treating AD. In particular, brain imaging for early AD detection is a highly active field of research.
Brain positron emission tomography (PET) scans produce detailed three-dimensional images of the inside of the brain and enables researchers to look for the presence of AD biomarkers in the brain, such as the beta-amyloid and tau proteins.
A study published in 2019 provided extensive data to support the use of amyloid PET scans in AD diagnosis and care.
In a new study, researchers at Lund University in Sweden, among other researchers from Australia, the United States, and the Netherlands, used PET imaging to investigate whether the presence of amyloid and tau proteins in the brain of cognitively healthy individuals is associated with future cognitive decline.
The results of the study appear in Nature Medicine.
Study co-author Rik Ossenkoppele, Ph.D., associate professor in translational neuroscience and principal investigator at the Alzheimercenter Amsterdam of the Amsterdam UMC and at Lund University, told Medical News Today:
“The study shows we can accurately predict the onset of symptoms in initially cognitively unimpaired individuals. Hence, cognitively unimpaired individuals with abnormal amyloid and tau PET scans need effective interventions to prevent future cognitive decline. Also, our findings provide support for a biological diagnosis of AD as defined by abnormal amyloid and tau PET scans.”
Amyloid and tau proteins as predictors of future cognitive decline
For the study, researchers recruited 1,325 cognitively unimpaired participants from 7 cohorts from Sweden, the U.S., the Netherlands, and Australia.
They used PET scans to check for the presence of amyloid and tau proteins in the participants’ brains and followed up on the participants’ cognitive health outcomes for an average of 3.5 years.
The results of the brain PET scans were as follows (‘+’ denotes presence and ‘-’ denotes absence; ‘A’ represents amyloid and ‘T’ tau proteins):
- 843 participants (63.6%) were A− T−
- 328 (24.8%) A+ T−
- 55 (4.2%) A+ TMTL+ (tau protein present in the medial temporal lobe)
- 65 (4.9%) A+ TNEO-T+ (tau protein present in the temporal neocortex)
During clinical follow-up, the proportions of participants who developed mild cognitive decline or dementia in the different AT biomarker groups were as follows:
- 26 out of 781 (3.3%) in A− T−
- 26 out of 292 (8.9%) in A+ T−
- 25 out of 51 (49.0%) in A+ TMTL+
- 32 out of 60 (53.3%) in A+ TNEO-T+
These findings showed A+ TMTL+ and A+ TNEO-T+ cognitively unimpaired individuals had a significantly higher risk for future development of mild cognitive decline and dementia.
The researchers also observed that the presence of amyloid and tau proteins was linked to short-term (that is, 3–5 years) cognitive decline in cognitively unimpaired individuals.
Implications for early detection of AD
Earlier this year, data from a Phase 3 clinical trial showed that the drug lecanemab slowed cognitive decline by 27%.
But before treatment is possible, diagnosis is necessary. It is a challenge to diagnose AD at an early stage because it takes about 10–20 years for biological changes in the brain to manifest as symptoms of cognitive impairment.
Based on the findings from the present study, the researchers hope that amyloid and tau PET scans may be used to identify individuals at risk of cognitive decline, enabling them to receive early effective interventions.
“If we can diagnose [AD] before cognitive challenges appear, we may eventually be able to use the drug to slow down the disease at a very early stage. In combination with physical activity and good nutrition, one would then have a greater chance of preventing or slowing future cognitive impairment”, Oskar Hansson, study co-author and professor of neurology at Lund University, said in a press release.
Christina B. Young, Ph.D., instructor in neurology and neurological sciences at Stanford University, noted to MNT that “the fact that amyloid and tau-positive individuals progressed to dementia in 4–4.5 years “provides a time frame for clinical trials to evaluate the effectiveness of their interventions.”
“These results also provide further evidence that A+T+ individuals may be the ideal target for secondary prevention trials as these individuals [are] likely to show clinical progression and cognitive decline even in a short-term (3–5 year) context.”
– Christina B. Young, Ph.D., neurology instructor
Study strengths and limitations in AD research
According to the researchers, the main strength of this study is its use of a large-scale multicenter dataset, which allowed an accurate estimation of the relative risk of cognitive decline in different AT groups.
In terms of study limitations, the researchers acknowledged that data collection was not perfectly harmonized across multiple cohorts. Additionally, the number of “events” (i.e., cognitively unimpaired individuals progressing to mild cognitive impairment or dementia) was relatively low.
Although Dr. Young commended the study findings, she pointed out the lack of diversity among participants.
“Recent studies have found differences in amyloid PET positivity between racial and ethnic groups, and it is unclear whether amyloid and tau have the same level and type of detrimental impact in non-white populations,” Dr. Young noted.
Dr. Bruno Dubois, professor of neurology at Pierre et Marie Curie University and director of the Institute for Memory and Alzheimer’s Disease (IM2A), who was not involved in this study, expressed caution about the study’s implications to MNT:
“Everyone agrees that the presence of positive [amyloid and tau] biomarkers increases the risk of a further progression to prodromal Alzheimer’s disease. This does not mean that these positive subjects will all develop the disease. We have already shown in a longitudinal study that not all individuals, by far, with positive biomarkers, progress to a clinical Alzheimer’s even after 7 seven years of follow-up.”
Professor Dubois added that disclosing the disease to people who may never develop it may be dangerous.
“Given the severity of the diagnosis, I think that we must remain very careful and maintain that these subjects are ‘at-risk’ and not that they have Alzheimer’s,” he said.
What’s next in Alzheimer’s research?
When asked about the next research steps, Dr. Ossenkoppele told MNT that future studies should:
Could PET screening for AD become widely available?
Dr. Ossenkoppele told MNT that PET scanning for AD is already happening at a “relatively large scale” for individuals with symptomatic AD (i.e., mild cognitive impairment of AD-type dementia).
“However, we focused in our study on cognitively unimpaired individuals, and in that population, this is highly unlikely to happen in the near future,” Dr. Ossenkoppele said.
“This may change when effective disease-modifying treatment becomes available in the future that is validated in this population and has an acceptable safety profile, but even then, more affordable, accessible, and scalable biomarkers (e.g., blood tests) would be the first step as PET is an expensive technique and its accessibility worldwide is limited.”
Source: Read Full Article