Using an artificial intelligence (AI) tool that emulates how humans visualize and is trained to recognize and classify images, investigators constructed a model that predicts the postoperative recurrence of Crohn disease with high accuracy by evaluating histological images. The AI tool also revealed previously unrecognized differences in adipose cells and significant differences in the extent of mast cell infiltration in the subserosa, or outer lining of the intestine, comparing patients with and without disease recurrence. The findings appear in The American Journal of Pathology.
The 10-year rate of postoperative symptomatic recurrence of Crohn disease, a chronic inflammatory gastrointestinal disease, is estimated at 40%. Although there are scoring systems to evaluate Crohn disease activity and the existence of postoperative recurrence, no scoring system had been developed to predict whether Crohn disease might recur.
“Most of the analysis of histopathological images using AI in the past have targeted malignant tumors,” explained lead investigators Takahiro Matsui, MD, Ph.D., and Eiichi Morii, MD, Ph.D., Department of Pathology, Osaka University Graduate School of Medicine, Osaka, Japan. “We aimed to obtain clinically useful information for a wider variety of diseases by analyzing histopathology images using AI. We focused on Crohn disease, in which postoperative recurrence is a clinical problem.”
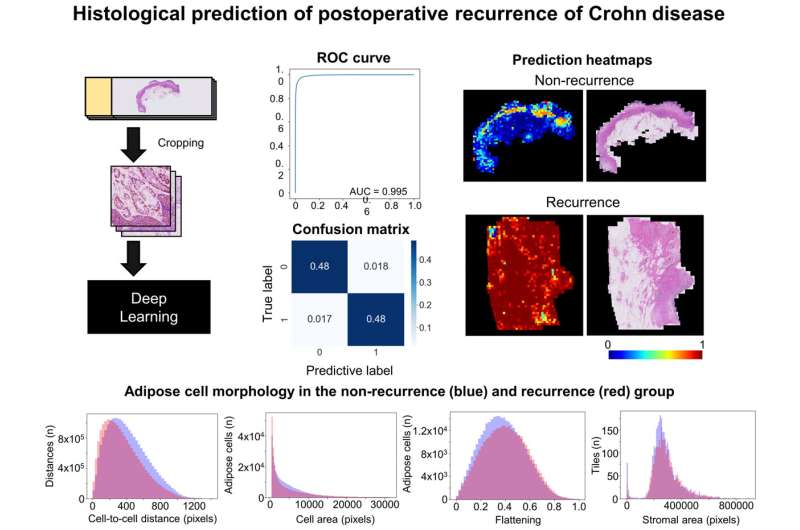
Sixty-eight patients with Crohn disease who underwent bowel resection between January 2007 and July 2018 were included in the study. They were classified into two groups according to the presence or absence of postoperative disease recurrence within two years after surgery. Each group was sorted into two subgroups, one for training an AI model and the other for validation. For training, whole slide images of surgical specimens were cropped into tile images, labeled for presence or absence of postsurgical recurrence, and then processed by EfficientNet-b5, a commercially available AI model designed to perform image classification. When the model was tested with unlabeled images, the results indicated that the deep learning model accurately classified the unlabeled images according to the presence or absence of disease occurrence.
Next, predictive heat maps were generated to identify areas and histological features from which the machine learning model could predict recurrence with high accuracy. The images included all layers of the intestinal wall. The heatmaps showed that the machine learning model yielded correct predictions in the subserosal adipose tissue layer. However, in other areas, such as the mucosal and proper muscular layers, the model was less accurate. Images with the most accurate predictions were extracted from the test datasets of the non-recurrence and recurrence groups. Among these images, the best predictive results all contained adipose tissue.
Because the machine learning model achieved accurate predictions from images of subserosal tissue, the investigators hypothesized that subserosal adipose cell morphologies differed between the recurrence and the nonrecurrence groups. Adipose cells in the recurrence group had a significantly smaller cell size, higher flattening, and smaller center to center cell distance values than those in the nonrecurrence group.
“These features, defined as ‘adipocyte shrinkage,’ are important histological characteristics associated with Crohn disease recurrence,” said Dr. Matsui and Dr. Morii.
The investigators also hypothesized that the differences in adipocyte morphology between the two groups were associated with some degree or type of inflammatory condition in the tissue. They found that the recurrence group had a significantly higher number of mast cells infiltrating the subserosal adipose tissue, indicating that the cells are associated with the recurrence of Crohn disease and the “adipocyte shrinkage” phenomenon.
Source: Read Full Article