As the coronavirus disease 2019 (COVID-19) pandemic persists worldwide, scientists have turned their attention to identifying better and faster methods to detect the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). In a new PLOS ONE study, researchers evaluate the accuracy of using dogs to smell and identify the presence of SARS-CoV-2 in infected and non-infected individuals.

Study: Diagnostic Accuracy of Non-Invasive Detection Of SARS-Cov-2 Infection by Canine Olfaction. Image Credit: Trudie Davidson / Shutterstock.com
Introduction
The need for a rapid and efficient method to screen for SARS-CoV-2 infected individuals has been recognized since the beginning of the outbreak. The early identification of these individuals allows for them to be quickly isolated to limit transmission of the virus and thus prevent the expansion of a localized outbreak.
While the reverse transcription-polymerase chain reaction (RT-PCR) assay has been the gold standard for the diagnosis of coronavirus disease 2019 (COVID-19), point-of-care testing with rapid antigen tests has also been implemented. In some places, salivary RT-PCR sampling replaced the traditional nasopharyngeal PCR tests to minimize the discomfort and inconvenience of nasopharyngeal swab sampling and the delay in getting the test results.
Volatile organic compounds in the human body show significant alterations in various disease states including cancers, as well as both infections and degenerative diseases. The levels of these VOCs are traceable to changes in the cellular genomic expression induced by the viral infection. These changes are specific and can be distinguished between infections with different strains of the same virus.
Dogs have been used to sniff out explosives, narcotics, currency notes, and human scents for search and rescue operations. In the current study, researchers report on the results of their experimental use of dogs to detect SARS-CoV-2 in sweat, which is presumably caused by virus replication or altered cellular metabolic processes.
Study findings
The current study used sweat samples from 335 participants in two COVID-19 screening programs at two centers in Paris, France. Some of the dogs were from French fire service departments, while the United Arab Emirates (UAE) Ministry of the Interior provided several more. All dogs were trained using the same methods that included both positive and negative smell cones.
The canine olfactory results were validated using nasopharyngeal and saliva RT-PCR results. Multiplexed detection of other viruses including adenovirus, endemic seasonal human coronaviruses like 229E and HKU1, influenza A H1 and H1N1, as well as some intracellular bacteria like Bordetella pertussis and Mycoplasma pneumoniae, was also performed.
The mean age of the participants was about 35 years. Most study participants were either symptomatic or were previously in contact with a COVID-19-positive individual. The median time between exposure or symptom onset to testing was five days and two days, respectively.
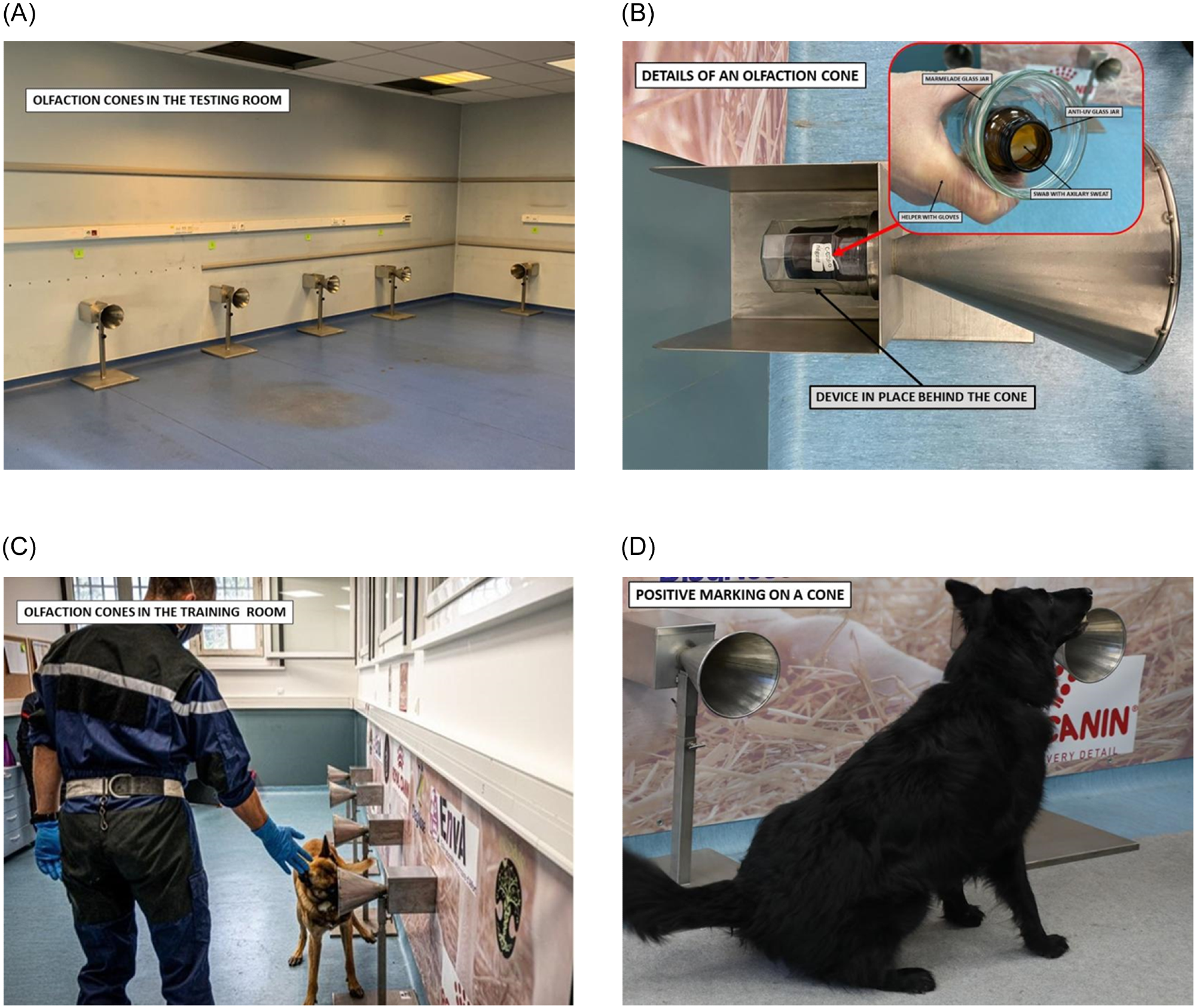 A: Testing room with its olfaction cones. B: Details of an olfaction cone, with a double-protected sample and no possibility of direct contact with the dog. C: Process involving olfaction cones and dog. D: Positive marking by a dog, sitting in front of a cone containing a positive sample.
A: Testing room with its olfaction cones. B: Details of an olfaction cone, with a double-protected sample and no possibility of direct contact with the dog. C: Process involving olfaction cones and dog. D: Positive marking by a dog, sitting in front of a cone containing a positive sample.
A third of the participants were positive for COVID-19 RT-PCR, 97% of whom were correctly detected by the dogs with a specificity of 91%. In fact, every asymptomatic individual was identified correctly by the dogs with a specificity of 94%. The sensitivity and specificity of this method compare favorably with that of nasopharyngeal and saliva RT-PCR with a cycle threshold (Ct) value of 32 as the cutoff and using one, two, or more target genes for a positive test.
Overall, 84% of positive identifications by the dogs were true positives, with the negatives identified correctly in almost every case. The accuracy of diagnosis did not change with prior treatment or history of prior infection. Whether the Ct value was set at 28 or less, or above this value, thus denoting high and low viral loads, respectively, no significant change in accuracy was found.
Different dogs were also associated with similar accuracies. The canine detection was more sensitive than the antigen tests at 91% and 84%, respectively; however, the dogs were associated with a lower specificity than the rapid antigen tests at 90% and 97%, respectively.
Out of 20 samples that were identified as positive by the dogs but were negative by multiplex RT-PCR, only one case was positive for SARS-CoV-2, while two were positive for endemic coronaviruses NL63 and OC43.
Implications
The findings of this study indicate “the excellent sensitivity of SARS-CoV-2 detection by dogs using nasopharyngeal RT-PCR as the reference for comparison.” This corroborates earlier proof-of-concept experiments on sweat samples from hospitalized COVID-19 patients. Notably, this is the first prospective screening study for SARS-CoV-2 infection that compares canine identification with antigen testing.
Interestingly, the sensitivity of the canine identification approach was greater than 95% in all scenarios, with specificity ranging between 83% and 95%. The comparable sensitivity with much higher convenience of sampling and much less patient discomfort could make this a viable option for screening tests.
Further research will be needed to determine if direct screening without the collection of sweat or saliva samples will yield comparable results. This could accelerate the current screening process considerably, though some individuals who fear dogs would have to be exempted. Moreover, contamination of the dogs is possible with this approach.
Some studies are already ongoing in this regard, especially among special needs children and patients with Alzheimer’s disease, both of whom are very difficult to sample. If successful, this testing approach could remove the need to routinely sample school children multiple times a week, as is the current practice.
However, trained dogs are expensive and in high demand, and their supply is limited. To ensure replicability of results, dog certification will also be required. Despite these potential limitations, the current study demonstrates the value of this method as an alternative to antigenic tests in terms of its convenience, speed, non-invasiveness, and reliability.
Further studies will be focused on direct sniffing by dogs to evaluate sniffer dogs for mass pre-test. Axillary sweat testing could remain useful for small population testing or for mobile units acting on local clusters as an alternative to antigenic tests.”
- Grandjean, D., Elie, C., Gallet, C., et al. (2022). Diagnostic Accuracy of Non-Invasive Detection Of SARS-Cov-2 Infection by Canine Olfaction. PLOS ONE. doi:10.1371/journal.pone.0268382, https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0268382
Posted in: Medical Science News | Medical Research News | Disease/Infection News
Tags: Adenovirus, Antigen, Assay, Bacteria, Children, Contamination, Coronavirus, Coronavirus Disease COVID-19, CT, Diagnostic, Diagnostics, Genes, Genomic, H1N1, Influenza, Intracellular, Mycoplasma, Narcotics, Nasopharyngeal, Olfaction, Pandemic, Pertussis, Polymerase, Polymerase Chain Reaction, Research, Respiratory, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Syndrome, Transcription, Virus

Written by
Dr. Liji Thomas
Dr. Liji Thomas is an OB-GYN, who graduated from the Government Medical College, University of Calicut, Kerala, in 2001. Liji practiced as a full-time consultant in obstetrics/gynecology in a private hospital for a few years following her graduation. She has counseled hundreds of patients facing issues from pregnancy-related problems and infertility, and has been in charge of over 2,000 deliveries, striving always to achieve a normal delivery rather than operative.
Source: Read Full Article





