Over the past two years, we have encountered numerous reports of persisting symptoms of Coronavirus disease (COVID-19), commonly referred to as "long COVID." These symptoms include breathlessness, fatigue, myalgia, hair loss, and diminished cognitive abilities.
Although the mechanisms and contributing factors for long COVID remain elusive, immunocompromised patients tend to partially sustain the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection.
There is evidence that antibodies specific to immunoglobulin A (Ig) are more effective against SARS-CoV-2 than antibodies specific to IgG, and represent a form of early potent neutralization. Both IgA and IgG antibodies are secreted in the breastmilk of nursing women who were previously infected by SARS-CoV-2 and in those who were vaccinated against COVID-19.
 Study: Clearance of Persistent SARS-CoV-2 RNA Detection in a NFκB-Deficient Patient in Association with the Ingestion of Human Breast Milk: A Case Report. Image Credit: Monthira / Shutterstock
Study: Clearance of Persistent SARS-CoV-2 RNA Detection in a NFκB-Deficient Patient in Association with the Ingestion of Human Breast Milk: A Case Report. Image Credit: Monthira / Shutterstock
The study
A new study published in the journal Viruses aimed to report the effects of plasma infusion and then breastmilk ingestion as a therapy for persistent SARS-CoV-2 infection in a patient with a common variable immunodeficiency (CVID) phenotype.
The patient selected had NFκB1 gene polymorphism, which is characterized by immunosuppression and severe B-cell and antibody production deficiencies.
Case Report
A 32-year-old female presented with a sore throat, cough, fever (38-38.5oC), along with headache, fatigue, anorexia, and diarrhea, on March 11, 2021, over the past two weeks.
A real-time quantitative polymerase chain reaction (RT-qPCR) of the nasopharyngeal sample elicited SARS-CoV-2 RNA.
On follow-up after one month, the patient was asymptomatic. Yet, the nasopharyngeal swab samples showed a viral load of 1.99 × 107 RNA copies per mL. Gene sequencing revealed the Gamma variant of SARS-CoV-2 as the causative organism.
Mild fever persisted for 75 days post-infection confirmation, and the patient also sustained weight loss over four months post-infection. Meanwhile, her chest tomography, electrocardiogram (ECG), and oxygen saturation (SpO2) levels remained normal. The other symptoms remained refractory during the post-COVID phase.
About three months after COVID diagnosis, 1.35 × 108 RNA copies/mL SARS-CoV-2 RNA were detected by real-time polymerase chain reaction (RT-PCR); genome whole-sequencing aided in confirming the result.
A maximum-likelihood phylogenetic analysis (with NextStrain) established Gamma lineage. The likelihood of reinfection was excluded.
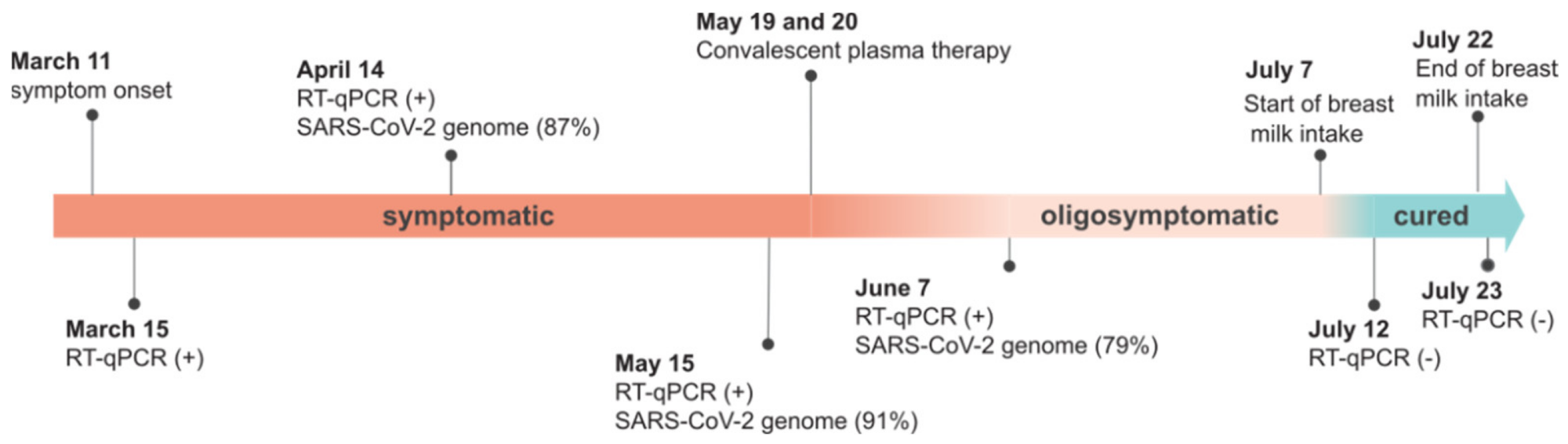 Timeline of COVID-19 in the NFκB-deficient patient. (+), positive; (−), negative. (%) represents the percentage coverage of the sequenced SARS-CoV-2 genome.
Timeline of COVID-19 in the NFκB-deficient patient. (+), positive; (−), negative. (%) represents the percentage coverage of the sequenced SARS-CoV-2 genome.
The patient was isolated and treated at home under medical supervision. Although this COVID-19 clinical course was deemed dysregulated, hyperinflammation was absent during 124 days post-diagnosis.
On May 19, 2021, the patient was given 600 mL of convalescent plasma with IgG titers: 1:640, intravenously from two COVID-19 patients – over two consecutive days. Three days post-infusion, her febrile illness disappeared, and the patient reported feeling better. At this time, SARS-CoV-2 RNA persisted in the oropharyngeal swab samples, as disclosed by an RT-qPCR test conducted on June 7, 2021.
Moreover, the patient had not fully recovered, her appetite had not returned, and she still felt weak. The asymptomatic infection remained, posing a risk for transmission and even progression into severe COVID-19.
Hereafter, ingestion of IgA specific for SARS-CoV-2 was suggested – derived from breastmilk of women who had received COVID-19 vaccination. This strategy was based on the finding that IgA dimers are more potent than IgG monomers in neutralizing SARS-CoV-2.
Pasteurized breastmilk from a BNT162b2-vaccinated (Pfizer–BioNTech) mother was utilized for this purpose––180 mL per day for two weeks. The intake was practiced such that the patient retains the milk in her mouth for at least three minutes before swallowing.
Just one week after the convalescent plasma infusion, the absolute neutrophils, lymphocytes, and monocytes doubled in numbers – which suggested hematopoietic recovery. However, the lymphocytes halved after a week––after the ingestion of the breastmilk––and showed a value of around the upper limit of the normal range.
The alterations in the above-mentioned parameters depicted the clinical status of the SARS-CoV-2 infection, which preceded the impact of the therapeutic interventions.
Of note, before the convalescent plasma infusion, the CD3+ and CD4+ cell numbers decreased by more than half of the usual numbers, which were reinstated post plasma infusion and breast milk ingestion. Yet, no changes were observed in the CD4+/CD8+ ratio or the absolute CD19+ count during the infection. While post-intervention, the significant reductions in the serum ferritin and C-reactive protein levels (which had earlier risen), hinted toward strong neutralizing activity––suggesting a protective effect.
The patient fully recovered by July 21, 2021; this was confirmed by negative test results (RT-qPCR) of oropharyngeal swab samples, 16 days post-therapy. On November 24, 2021, the patient remained COVID-19 negative – according to IgM non-reagent and RT-qPCR tests.
This case report marks an unconventional use of specific secretory antibodies from human breastmilk as a therapy against COVID-19. It was speculated that the IgA antibodies secreted in breastmilk of COVID-19 vaccinated women can neutralize SARS-CoV-2 sustained in various organs of the recently infected individuals, such as – the tonsils, oropharynx, and gastrointestinal tracts.
Hence, such therapeutic intervention can aid in the clearance of infection in immunodeficient individuals with long COVID. In the present case, any new mutations in the Gamma variant genome or single nucleotide polymorphisms (SNPs) were not observed during the entire study period despite the patient being immunodeficient.
- Sabino, J., Amorim, M., de Souza, W., et al. (2022). Clearance of Persistent SARS-CoV-2 RNA Detection in a NFκB-Deficient Patient in Association with the Ingestion of Human Breast Milk: A Case Report. Viruses. doi: 10.3390/v14051042. https://www.mdpi.com/1999-4915/14/5/1042
Posted in: Medical Research News | Women's Health News | Disease/Infection News
Tags: Anorexia, Antibodies, Antibody, Breast Milk, CD3, CD4, Cell, Convalescent Plasma, Coronavirus, Coronavirus Disease COVID-19, Cough, covid-19, C-Reactive Protein, Diarrhea, Fatigue, Fever, Gene, Gene Sequencing, Genome, Hair, Hair Loss, Headache, Immunodeficiency, Immunoglobulin, Immunosuppression, Nasopharyngeal, Neutrophils, Nucleotide, Nursing, Oxygen, Phenotype, Polymerase, Polymerase Chain Reaction, Protein, Respiratory, RNA, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Single Nucleotide Polymorphisms, Sore Throat, Swallowing, Syndrome, Throat, Tomography, Weight Loss

Written by
Nidhi Saha
I am a medical content writer and editor. My interests lie in public health awareness and medical communication. I have worked as a clinical dentist and as a consultant research writer in an Indian medical publishing house. It is my constant endeavor is to update knowledge on newer treatment modalities relating to various medical fields. I have also aided in proofreading and publication of manuscripts in accredited medical journals. I like to sketch, read and listen to music in my leisure time.
Source: Read Full Article




