The small size of a new study of the feasibility of tapering conventional synthetic disease-modifying antirheumatic drug (csDMARD) doses to half for patients with rheumatoid arthritis (RA) in remission, and then to zero, makes suspect the validity of its finding of no statistical difference between continuing half doses and stopping altogether, according to one rheumatologist’s analysis.
In the open-label, randomized trial of 56 patients, which was published as a research letter in JAMA on March 28, more patients in the group that discontinued csDMARDs experienced flares within 1 year than did the half-dose group, but this difference was not statistically significant.
Most patients in the drug-free group did not experience disease flares, the authors note.
“The results show that in this population, a majority of patients remained flare-free for at least a year after csDMARD discontinuation. This highlights a potential for drug-free remission in a subgroup of RA patients, and the data provide a basis for shared decision-making in this patient group. We know that tapering is a common question from patients, and thus think that the data are especially clinically relevant,” first author Siri Lillegraven, MD, MPH, PhD, of the Center for Treatment of Rheumatic and Musculoskeletal Diseases at the Diakonhjemmet Hospital in Oslo, Norway, said in an interview with Medscape Medical News.
While several studies have demonstrated that patients with RA can maintain remission on lower doses of medication, James O’Dell, MD, chief of the Division of Rheumatology at the University of Nebraska Medical Center in Omaha, urged caution in interpreting these results because the study was so small ― just 56 patients. “Every analysis they did favored staying on treatment, but the confidence interval slightly crossed null, so they can’t say [that group] was superior,” O’Dell told Medscape. He was not involved in the research. “Had this study been double this size and they got the same results, they would have clearly shown that staying on medicines were superior,” he said.
Lillegraven acknowledged the impact of the trial’s small sample size. “This is a study with a limited study sample, and it is conceivable that a larger study might have shown a statistical difference between the groups,” she said.
In addition to the small number of patients in the study, O’Dell also noted that this study group was already a selected group of patients who had maintained remission on half-dose therapy for at least 1 year. Even then, “what they showed was that 39% of the patients who they discontinued [then] flared, compared to 17% when they didn’t taper [off medication],” he said. “That’s a pretty important clinical difference.”
While O’Dell thinks the study was too small to inform practice, he emphasized that tapering off full doses of medications can be beneficial for patients with RA that has been in remission for 6 months or longer. “It seems to take less medicines to keep somebody in remission than it did to get them there in the first place,” he said. “I come out strongly in favor of tapering medications in rheumatoid arthritis patients who are in remission, and that includes tapering and stopping biologics if patients are on conventional therapy,” he added, “but tapering patients off all of their conventional therapy is something that I think is a bridge too far.”
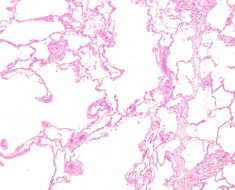
This trial was the second part of the ARCTIC REWIND study, which involved patients with RA that was in sustained remission, per their Disease Activity Score. In the first part of the trial, 160 participants from 10 hospitals in Norway were enrolled and were randomly assigned to either continue their standard csDMARD dosing or taper down to a half dose. Patients whose doses were tapered to a half dose and whose conditions were in remission for 1 year were eligible for the second half the study.
Of the 56 participants who were included, 26 discontinued csDMARD therapy, while 30 continued taking a half dose for 12 months of follow-up. Most patients in both groups had received methotrexate monotherapy (21 in the discontinuation group and 26 in the continued half-dosing group). Triple therapy (methotrexate, sulfasalazine, and hydroxychloroquine) was used by three patients in the discontinuation group and by two in the half-dose group. Two additional patients in the discontinuation group and two in the half-dose group took other mono/duo therapies. Clinic visits occurred every 4 months; visits were more frequent if there was an increase in disease activity. For patients who experienced a disease flare, full-dose csDMARD treatment was resumed.
Ten patients in the discontinuation group experienced flares during 1 year, compared with five patients in the half-dose group. The risk difference (RD) between the two groups was not statistically significant (RD, 21.5%; 95% CI, -3.4% to 49.7%). The median time to flare was 179 days in the discontinuation group and 133 days in the half-dose group.
Of those who experienced flares, 8 of 10 patients in the discontinuation group and 2 of 5 in the half-dose group regained remission when full-dose therapy was resumed.
The study was funded by the Research Council of Norway and the South-Eastern Norway Regional Health Authorities. Many of the authors disclosed financial ties to pharmaceutical companies. O’Dell disclosed no relevant financial relationships.
JAMA. Published online March 28, 2023.
For more news, follow Medscape on Facebook, Twitter, Instagram, and YouTube.
Source: Read Full Article