Studying the mutations in kidney cancer after surgery could help to better predict the risk of the disease coming back, according to the latest results of a decade-long international study.
The research, undertaken by a team of 44 researchers at 23 institutions across Europe and Canada, including McGill University, is the largest to link the genetic changes that occur in kidney cancer to patient outcomes.
More than 400,000 people are diagnosed with kidney cancer each year globally, including 8,100 in Canada and 81,800 in the United States.
Our research shows that it may be possible to improve the way we determine risk in each patient by looking at the genetic mutations present in their cancer."
Yasser Riazalhosseini, Assistant Professor of Human Genetics, and Head of Cancer Genomics at the Victor Phillip Dahdaleh Institute of Genomic Medicine, McGill University
"Mutation analysis using DNA sequencing is already being used to help patients with other types of cancer and could be readily applied to patients with kidney cancer," he adds.
The study published today by the University of Leeds and McGill University, looked at changes in the DNA of more than 900 of kidney cancer samples, and identified four groups of patients based on the presence of mutations in 12 specific genes within the DNA. The team also looked at whether the cancer had recurred in each of these patients.
The researchers found some 91 per cent of patients in one mutation group remained disease-free five years after surgery, meaning patients in this group may potentially avoid unnecessary treatment. Meanwhile, the percentage of patients in a different mutation group who remained disease-free at five years was much lower, at 51 per cent. This identified them as requiring more aggressive treatment.
Preventing cancer recurrence
Cancer Research eBook

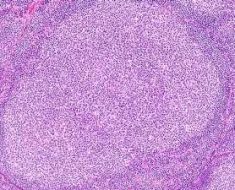
Currently, doctors assess the risk of kidney cancer returning by looking at features like the size of the tumor and how aggressive it appears under a microscope. With up to 30 per cent of localized kidney cancers returning after surgery, more accurate methods of assessing this risk are needed, meaning patients who do not need further treatment can be spared it, say the researchers.
"Accurately determining the risk of cancer recurrence is very important. It helps us identify how often patients need to be seen by their doctors and decide who to treat with immunotherapy. This treatment has recently been shown to reduce the chances of the cancer coming back but can cause side-effects. The danger currently is that some patients may be over-treated, so being able to better identify patients at low risk of recurrence is important," says Naveen Vasudev, Associate Professor and Honorary Consultant in Medical Oncology at the Leeds Institute of Medical Research.
Personalizing risk prediction and treatment
The results of this research mean that tumor DNA sequencing may provide a more effective way to predict a patient's risk of kidney cancer recurrence. This could, in the future, lead to more personalized treatment for kidney cancer.
"Development of new treatments for kidney cancer has lagged behind other cancers and we largely continue to adopt a 'one size fits all' approach," says Vasudev.
"Genomics – the study of genes and how they interact with each other – is a key area of development in patient care. Here we show how genomics might be applied to patients with kidney cancer, potentially creating more personalized treatment options for thousands of patients each year," he says.
McGill University
Vasudev, N.S., et al. (2023) Application of Genomic Sequencing to Refine Patient Stratification for Adjuvant Therapy in Renal Cell Carcinoma. Clinical Cancer Research. doi.org/10.1158/1078-0432.CCR-22-1936.
Posted in: Genomics | Medical Condition News
Tags: Adjuvant Therapy, Cancer, Carcinoma, Cell, DNA, DNA Sequencing, Genes, Genetic, Genetics, Genome, Genomic, Genomic Sequencing, Genomics, Immunotherapy, Kidney, Kidney Cancer, Medical Research, Medicine, Microscope, Mutation, Oncology, Renal Cell Carcinoma, Research, Surgery, Tumor
Source: Read Full Article