DR MICHAEL MOSLEY: They’re responsible for 80% of cases and are the key to stopping corona. No wonder scientists are racing to work out… how to stop a superspreader (clue: they look like Trump)
With Covid cases on the rise, it’s clearly very important to identify what’s driving this second wave. Is it students socialising at university? Or is it people packing into bars?
It’s probably a bit of both, but there is mounting evidence that the main driver is a small group called ‘superspreaders’.
They may not have symptoms but still manage to infect lots of others. In reality, relatively few people are responsible for the majority of cases.

The researchers also showed the people who produced the most droplets (i.e. the potential superspreaders) tended to be older, with a higher BMI (body mass index). In other words, someone like Donald Trump. This group are not only more vulnerable to the virus, but it seems more prone to spread it if infected
A striking example of a superspreader was 53-year-old Steve Walsh, who at the start of the UK outbreak managed to unknowingly infect at least 11 others.
He got infected at a conference in Singapore and then went skiing. He infected most of the people in his chalet but what was surprising is they didn’t then go on to infect many others.
In fact, a nine-year-old boy in the party who later tested positive for the virus, did not pass it onto anyone else, despite coming into close contact with more than 170 people over the following days before he was identified.
This is not a fluke. It seems that 80 per cent of new cases are caused by just 10 per cent of infected people — most people who get Covid-19 never give it to anyone else.

A striking example of a superspreader was 53-year-old Steve Walsh, who at the start of the UK outbreak managed to unknowingly infect at least 11 others
If we can identify the superspreaders and isolate them quickly, it could have a big impact on the spread of Covid.
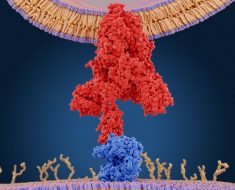
So is there something unusual about the people who become superspreaders? In a fascinating experiment, researchers from Harvard University in the U.S. took 74 healthy volunteers and measured their breath over two days, counting how many tiny droplets they breathe out.
They found seven individuals, ie roughly 10 per cent, who produced far more droplets than the others.
The researchers also showed the people who produced the most droplets (i.e. the potential superspreaders) tended to be older, with a higher BMI (body mass index). In other words, someone like Donald Trump.
This group are not only more vulnerable to the virus, but it seems more prone to spread it if infected. So, beyond the fact that they’re likely to be older and heavier, how can you identify a superspreader?
At the moment the only way is with track and trace. This means doing lots of testing and then tracking back contacts to see who’s been doing the infecting.
While researching my recent book on the coronavirus, I came across the story of the original superspreader, ‘Typhoid Mary’, who seeded outbreaks of typhoid fever in New York and other parts of the U.S. in the early 1900s.
Typhoid, which is caused by a salmonella infection, used to be a major killer in crowded cities until sanitation improved.
During an outbreak in New York in 1907, the daughter of a rich industrialist died and he hired a researcher to find out why. This researcher discovered that a woman called Mary Mallon who’d worked as a cook in their house had also worked in other houses where people had subsequently got typhoid.
Although Mary had no symptoms, when doctors examined her poo it had lot of salmonella bacteria. Mary was a carrier, and in a time before antibiotics, there was nothing to cure her.
To protect the public she was confined to a hospital bungalow for three years and then released on condition she never worked as a cook again. But she just changed her name and went on working.
She was finally caught, a few years later, cooking in a hospital where a typhoid outbreak led to 25 people being infected, and two dying. Mary was arrested and confined until her death, 23 years later.
To our modern sensibility this is inhumane, but clearly the major difference is that isolating a Covid superspreader would last days, perhaps weeks, not years — if track and trace can spot them.
But rather than identifying individuals, the key may lie in reducing superspreader events. These are one-off gatherings where lots of people get infected.
It could be a pub, like the one in Aberdeen where 13 people tested positive; or a chummy meeting of Right-wing U.S. politicians, presided over by Donald Trump, which led to seven cases.
Central to the idea of superspreader events is a new understanding about the virus — just as important as the R rate (how many people someone typically infects), is the ‘K value’.
This is the pattern in which the virus spreads. With infections such as flu, the K value is one — it spreads evenly, each infected person typically passing it on to one other.
The K value for Covid is lower — around 0.1 — suggesting a small number of people cause most infections.
And where are you likely to meet these superspreaders?
Essentially, in crowded indoor spaces that are badly ventilated, filled with noisy strangers in close proximity, spraying lots of viruses around.
On that basis, planes, cinemas, restaurants and theatres are pretty safe; while busy pubs and bars, particularly where there are lots of people shouting and laughing, are best avoided.
This may help explain some of the thinking behind the recent introduction of new lockdowns.
Years ago on a visit to Iceland I decided to try a local delicacy, fermented fish. But the smell was so strong I found it almost impossible not to gag, let alone scoff it down. Icelanders enjoy such delicacies because it’s part of their culture, like the French with their smelly cheeses. But a new study in the journal Current Biology suggests there’s also a possible genetic explanation.
It seems a surprisingly high number of people in Iceland have a mutant version of the gene that allows most of us to detect rotten fish and avoid it — the mutation means they don’t mind the smell, but actually find it quite pleasant, describing it as sugary or floral!
The first thing I do when I get out of bed in the morning is my resistance exercises — five minutes of press-ups and squats. I find that if I don’t do them then, I don’t do them at all.
Then I stagger downstairs for a cup of tea, followed by an early-morning walk, if I have time, then a cup of coffee before breakfast. My wife Clare prefers to save her caffeine hit for later in the morning. So who is right?
Well, a new study from the University of Bath suggests Clare is — it seems drinking coffee before breakfast disrupts blood sugar levels in a way it doesn’t if you have your coffee afterwards.
Another reason why you might want to delay your coffee is that we all experience a brief surge in the hormone cortisol around the time we wake up, which jolts us into life.
Cortisol is a stress hormone, but it also signals the body to wake up. Levels typically peak around 8.30am, so if you add caffeine on top of that you may actually undermine its effectiveness.
Better to wait until at least 9.30am, when cortisol begins to dip, before giving yourself a caffeine hit.

I stagger downstairs for a cup of tea, followed by an early-morning walk, if I have time, then a cup of coffee before breakfast. My wife Clare prefers to save her caffeine hit for later in the morning. So who is right? [File photo]
Source: Read Full Article