Employment for frontline healthcare workers should be conditional on COVID-19 vaccination, and unless they have a valid medical reason for not getting the jab, persistent refusniks should be temporarily redeployed to protect their colleagues and patients, argue ethicists in the Journal of Medical Ethics.
The ramifications of not getting vaccinated, coupled with the seriousness of COVID-19, justify at the very least, a mild form of mandatory vaccination policy, they contend.
It’s an idea currently being considered by the UK government: last month it launched a 6-week public consultation on whether to require all older adult care home providers to make a COVID vaccination a condition of employment for their staff.
Experience of the seasonal flu jab shows that coercive approaches to vaccination uptake effectively increase uptake among healthcare workers and reduce the numbers of patients getting sick–if properly implemented–say the authors.
But overly coercive regulation might undermine goodwill between frontline healthcare staff and their employers, and promote resentment, opposition, and mistrust, particularly as these workers already experience higher rates of depression, anxiety, insomnia, post-traumatic stress disorder and burn-out from dealing with the tragic reality of this pandemic, note the authors.
Therefore, any policy needs to strike a fine balance between the various ethical principles at stake, they emphasize.
“From an ethical perspective, what matters is that the collective benefits outweigh the risks, and that there is some limit to the kind of risks that can be imposed for the sake of those collective benefits,” they write.
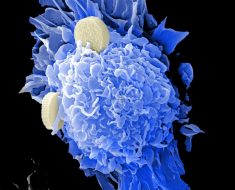
Using the principle of least restrictive alternative, they therefore developed an ‘intervention ladder’ for COVID-19 vaccination policies for frontline healthcare workers–all those with direct patient contact: doctors, nurses, allied health clinicians, pathology staff, security staff, cleaners and students.
From least to most coercive, the range of options might include:
- Education campaigns or professional development activities to persuade frontline healthcare workers to reconsider.
- Opt-out policies, such as requiring frontline healthcare workers to sign a statement explaining why they are refusing COVID-19 vaccination; reporting vaccination rates across different teams and highlighting underperforming teams in a bid to increase rates
- No access to employee privileges, such as additional paid leave; no access to restricted areas such as tea rooms or health clubs; no professional registration fee discount.
- Redeployment to non-clinical duties, working from home. Restricted direct clinical work with elderly, vulnerable, immunocompromised patients.
- Employment suspended; enforced leave; loss of salary for days not worked; admitting rights suspended; conditions imposed on professional registration preventing frontline healthcare work.
- Fines or imprisonment; termination of employment; cancellation of professional registration.
- Forcible vaccination using chemical or physical restraint, if required.
While frontline healthcare workers can choose between vaccination and their job, patients can’t choose whether or not to get sick nor who cares for them when sick. They might have no alternative but to be treated and cared for by unvaccinated staff, note the authors.
Therefore, the restriction on choice experienced by sick patients if no mandatory vaccination is imposed on frontline healthcare workers could be greater than the restriction experienced by staff if such a policy is imposed, they argue.
“Within healthcare settings, vaccine choices can have even greater ramifications, which, when coupled with the seriousness of COVID-19, justifies at least a mild form of mandatory vaccination policy for [frontline healthcare workers].
“We believe that this should take the form of conditional employment or conditional professional registration, although temporary redeployment could be adopted if this does not entail significant costs to patients, to vaccinated colleagues and to the healthcare system,” they write.
“This ’conditional’ policy is a compromise between entirely voluntary or entirely mandatory policies for healthcare workers, and is consistent with healthcare workers’ established professional, legal, and ethical obligations to their patients and to society at large,” they point out.
“In our view, this strikes the best balance between the various ethical principles at stake,” they conclude.
BMJ
Bradfield, O.M & Giubilini, A., (2021) Spoonful of honey or a gallon of vinegar? A conditional COVID-19 vaccination policy for front-line healthcare workers. Journal of Medical Ethics. doi.org/10.1136/medethics-2020-107175.
Posted in: Disease/Infection News
Tags: Anxiety, Burn, Consultation, Depression, Education, Flu, Healthcare, Insomnia, Pandemic, Pathology, Post-Traumatic Stress Disorder, Stress, students, Tea, Vaccine
Source: Read Full Article