Engineered human capillaries are providing an astounding view of how red blood cells transit ultra-small blood vessels.
This new platform was used in a recent study to learn how severe malaria infection causes red cells to get stuck in blood microvessels. As they accumulate, the parasite-infected red cells obstruct the narrowest routes of blood flow in the body.
The way the 3-D microvessel model was created with living cells, and the findings it helped glean on the mechanisms of microcirculatory obstruction by severe malaria infection, are reported in a paper in the current issues of Science Advances.
Researchers at the University of Washington, Seattle Children’s Research Institute, and the UW Medicine Institute for Stem Cell and Regenerative Medicine conducted the project.
The corresponding authors of the resulting paper are Ying Zheng, associate professor of bioengineering, Joseph D. Smith, affiliate professor of global health and a Seattle Children’s infectious disease researcher, and Cole A. DeForest, assistant professor of chemical engineering and bioengineering
The 3-D capillary system their team developed holds promise for research on several other diseases that cause blockage or damage to human capillaries. These include sickle cell anemia, diabetes, and cardiovascular problems.
The system might also be an initial step toward engineering microcirculation for regenerative medicine purposes, such as to supply sufficient blood flow to organ-repairing patches derived from stem cells or to laboratory-grown organs.
In the human body, capillaries are the smallest blood vessels. They are important conduits for the transfer of oxygen and nutrients from the blood stream to tissues, in exchange for carbon dioxide and waste products.
Human capillaries are so narrow that red blood cells pass through them one-by-one.
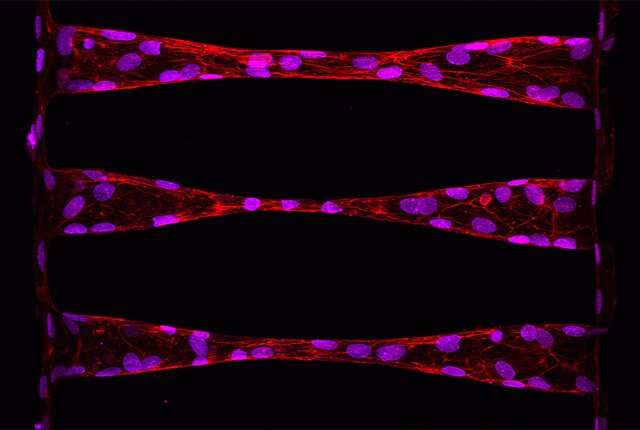
The scientists were able to construct their capillary system through a type of biological printing of vessels 100 micrometers in size engraved into a collagen base. Multiphoton technology from the DeForest lab was employed to etch the channels and to disturb cells from larger blood vessels, thereby encouraging them to move into the channels and form capillaries.
With their 3-D engineered microvessel, which resembles an hourglass, the scientists could analyze how red blood cells navigate tight bottlenecks. Normal red blood cells, which are shaped like a round rubber raft, get through smoothly by contorting themselves to look like slippers, parachutes or bells. They somehow seem to avoid touching the inside of the capillary.
However, red blood cells infected with malaria are more rigid and knobby. When transversing the capillary region, they do not elongate very much. They also roll and tumble. Both their shape and motion increase their risk of adhering to the capillary and becoming trapped.
Encountering the forces present in blood flow, infected red blood cells tend to be pushed more toward the capillary wall compared to their uninfected counterparts. This shoving aside also raises their likelihood of sticking.
While most normal red blood cells passed through the narrowest regions of the capillary model without a hitch, those infected with certain malaria parasite variants steadily accumulate. Within minutes they can dam the capillary and stop the flow, trapping some normal red blood cells with them.
The researchers performed additional analysis of the possible detrimental contributions of the knobs that appear on malaria-infected red blood cells.
They concluded that the dynamic forces of blood flow on the infected cells, and the modifications in the red blood cells induced by the malaria parasite might play independent roles in the events leading to blockage of microvessels. So, for example, there is more gathering of infected cells near the exit from the capillaries, which is the spot where blood flow slows down and shear stresses are reduced.
The scientists mentioned that two possible shortcomings of their 3-D human microvessel model is that it was derived from cell types originating in larger blood vessels and that studying single-cell dynamics is challenging due to imprecise flow control.
Source: Read Full Article





