England recently emerged from a four-week lockdown into a series of tiered restrictions, and there is good news about the authorisation of the first vaccine for COVID-19, which is starting to be deployed. But with restrictions loosened, infection rates still high and vaccine deployment slow, is there a risk of a third lockdown in early 2021?
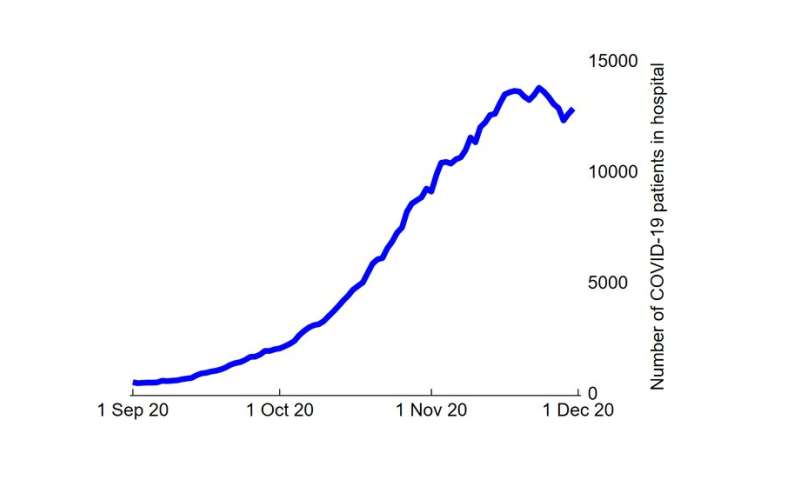
The second English coronavirus lockdown has been devastating for businesses in retail and hospitality. Yet we can see the lockdown has “worked,” bringing case numbers down almost by half from their peak. Rates of new admissions to hospital have also fallen, but pressure on England’s National Health Service (NHS) has not eased substantially.
The number of patients in hospital for COVID-19 has little more than flattened during November, providing hardly any additional capacity to manage the combined impact of loosening restrictions and normal winter pressures on the NHS.
A key difference between this second wave of COVID-19 in England and the first wave in March and April is that the NHS is trying to continue normal services—such as life-saving cancer and heart surgery—as much as possible. So what does life in the NHS during winter usually look like, and what capacity is there to manage more than 10,000 COVID-19 patients in hospital at one time alongside usual care?
End of winter struggle
The winter months are a high-pressure period for the NHS at the best of times. Lower temperatures are associated with a higher rate of hospital admission from emergency departments, and patients often need to stay in hospital longer, both of which increase bed occupancy rates. Older patients with respiratory conditions and other underlying conditions are most affected by a consistent low temperature, even when winter is less severe.
Increased pressure is reflected in a decline in performance for key patient-flow targets, such as the proportion of patients admitted, transferred or discharged from the emergency department within four hours. This seasonal spike in pressure can be expected on top of longer-term demographic trends leading to more emergency department attendances of patients with more complex health needs.
Intensive care units (ICUs) in England also operate at a high level of occupancy during winter months. Between December 2019 and February 2020, occupancy in adult ICU averaged 82% of the 3,730 ICU beds, leaving only about 670 spare at any time. The current number of COVID-19 patients in ICU in England (as of late November) is more than 1,500. While the Nightingale hospitals have given the NHS increased capacity to treat COVID-19 patients, and usual winter pressures caused by influenza might be mitigated by social distancing, the picture is still far from comforting.
In past years, hospitals have responded to winter pressures by delaying elective procedures to free up capacity. This approach comes on top of both a general recent trend for patients to wait longer for elective procedures and cancer treatment. It also suggests there is less flexibility to respond to an increase in COVID-19 cases in the same way than there was during the summer months.
Effect of vaccines will take time
While it’s great news that vaccines are being administered for the first time this week, several factors work against vaccines relieving pressure on the NHS any time soon. First, the UK only has access to very limited quantities of vaccines to begin with and will be using them slowly over the final weeks of December and into January. Second, these vaccines take between two to four weeks to build immunity in those immunized.
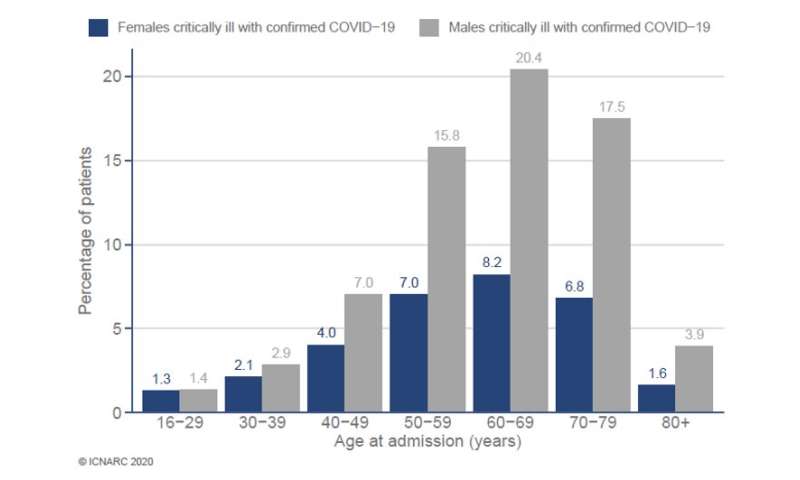
Finally, and most importantly, vaccines are being prioritized to those at most risk of death—initially the over-80s, rather than those who make up the highest number of patients in ICU with COVID-19 – people in their 50s, 60s and 70s. Half of the patients in ICU with COVID-19 are under 62 years of age. It may take many months before a large number of these “middle-aged” people have been successfully immunized, relieving pressure on ICUs.
Pressures may start to show by end of January
The tier system that replaced the lockdown in England is tougher than the pre-lockdown (October) version. For example, tier 2 (high risk) in the new system broadly equivalent to the previous tier 3. However, there remains a high degree of uncertainty about how effective the tiers are at reducing or controlling case numbers.
The government has also decided to relax restrictions over the Christmas period to allow more household mixing, which seems likely to lead to an increase in infections in early January. By mid to late January, the increased infections from the Christmas period will have had an impact on new hospital admissions and gradually started to increase the number of patients in hospital with COVID-19.
Source: Read Full Article