Researchers from the Institute of Process Engineering (IPE) of the Chinese Academy of Sciences, Beijing Chaoyang Hospital and the University of Queensland have developed a new formulation based on regulatory T-cell exosomes (rEXS) to deliver vascular endothelial growth factor (VEGF) antibodies for choroidal neovascularization therapy.
The study was published in Nature Biomedical Engineering on July 26.
Ocular neovascularization is often associated with age-related macular degeneration, diabetic retinopathy and other ocular diseases, which can cause severe vision loss.
The present treatment for ocular neovascular disease in clinic is intravitreal injection of VEGF antibodies (aV) to block the activity of VEGF and suppress pathogenic angiogenesis. However, this therapy alone faces problems of fast metabolism with the aqueous humor, poor accumulation in lesions and limited efficacy. A considerable proportion of patients still show incomplete response to above aV treatment.
In this study, the researchers collected aqueous humor samples from a large cohort of patients and quantified VEGF and other proinflammatory cytokines. “We observed a strong association between inflammation and high VEGF expression in aqueous humor samples,” said Prof. Tao Yong from Beijing Chaoyang Hospital. Thus, they proposed a synergistic therapeutic approach that combines anti-VEGF and anti-inflammatory therapies.
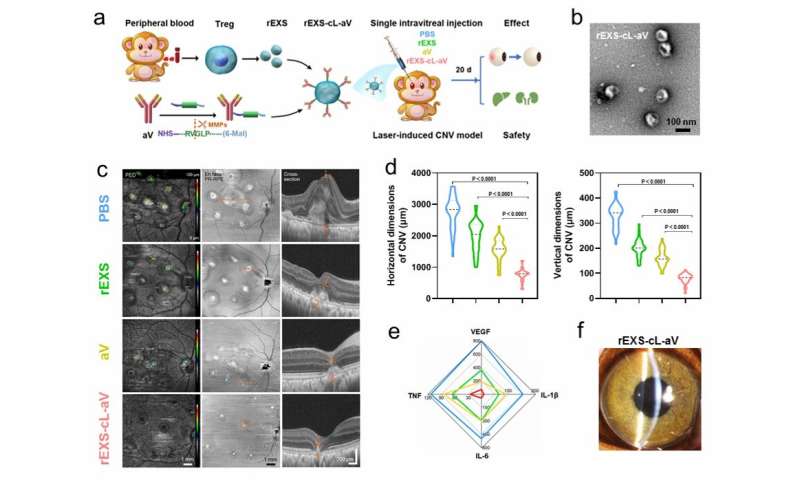
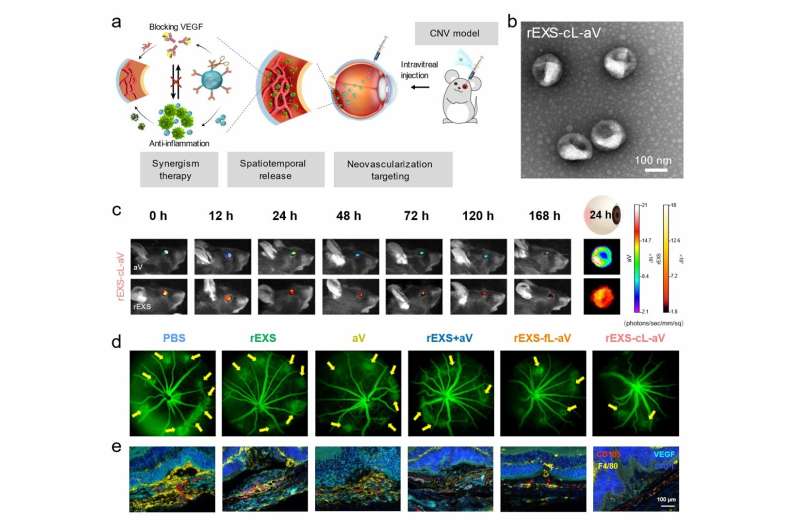
Following this approach, exosomes isolated from regulatory T-cells were utilized to conjugate aV using a peptide linker (cL), which was subject to cleavage by matrix metalloproteinases (MMPs) in inflammatory lesions. “This design concept could achieve efficient spatiotemporal delivery for combination therapy. After intravitreal injection, rEXS-cL-aV exploited the ability of rEXS to localize in neovascularization lesions and, upon MMP-mediated cleavage, released rEXS and aV to suppress inflammation and VEGF activity, respectively,” said Prof. Wei Wei from IPE.
The potent therapeutic efficacies were confirmed in both murine and nonhuman primate models of choroidal neovascularization. “This study is still at the preclinical stage. Given that rEXS can be produced from the patients’ own cells and aV has been approved for clinical use, our rEXS-cL-aV has the potential for translation to clinic,” said Prof. Yu Di from the University of Queensland.
Source: Read Full Article