- In some people with COVID-19, an overreaction of their immune system can damage their lungs.
- An anti-inflammatory drug may help reduce this damage and keep them off a ventilator.
- The Food and Drug Administration has also given the green light to clinical trials of compounds that were still being studied for use in other conditions.
The rise of COVID-19 has led to a scramble for ventilators to help the sickest patients. Now experts are hoping experimental drugs may help treat some of these patients before they need help breathing.
For some people who need ventilators, it’s not the virus that’s ravaging their lungs but their own immune system.
In some people, the immune system goes into overdrive.
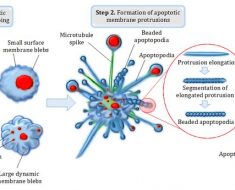
A new paper published today in the Journal of Experimental Medicine found that overactive white blood cells known as neutrophils may start to attack the lungs and other organs after mistaking the tissue for pathogens.
As the body’s immune system starts to attack, this process, called a “cytokine storm,” becomes dangerous and can cause more damage than the virus itself.
Cytokines are proteins that help the immune system fight an infection. These molecules are responsible for common symptoms of influenza, such as aches, fever, and inflammation.
However, when cytokines are out of control, they can make you even more sick. In some cases, the cytokine storm is fatal.
Scientists suspect that excess cytokines released by the immune system may be responsible for the lung damage and acute respiratory distress syndrome (ARDS) seen in certain people with COVID-19.
Several anti-inflammatory drugs are already being studied to see whether they can quell this cytokine storm, lessen the lung damage, and keep people off ventilators.
Treating overreaction of immune system
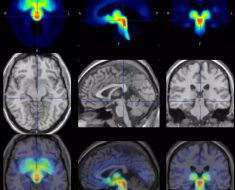
Ventilators help people with damaged lungs breathe, buying them time until another treatment allows their body to heal.
These machines, though, are in short supply in many hospitals. This shortage is worsened by COVID-19 patients on ventilators needing to be on the device longer than people with other conditions.
People with COVID-19 who are on a ventilator also have an increased risk for dying. A study published last month in the New England Journal of Medicine found that around 50 percent of these people die.
It’s not clear why the death rate is so high.
It could be that by the time people need help breathing, their disease is already more severe. The breathing tube used in the ventilator can also allow other germs to enter the lungs, causing an infection.
The cytokine storm may also be involved. This immune overreaction can damage not only the lungs, but also the kidneys and other organs. Once that damage is too far along, people are less likely to recover.
Dr. Randy Cron, an immunologist at the University of Alabama at Birmingham, says that in people hospitalized for COVID-19, a subset of patients — including those under 60 years old — develop cytokine storm syndrome as part of the infection.
For these people, “in addition to treating the virus, the cytokine storm syndrome also needs to be treated,” he said, “although we still don’t know what will work at this point.”
Cron says therapies that target inflammatory cytokines in people hospitalized for COVID-19 could reduce deaths and admissions to the intensive care unit (ICU).
“Hopefully, this would cut down on ventilator and healthcare worker needs,” he said.
The key is to reduce cytokine levels early on.
“We need to screen early among hospitalized COVID-19 patients so therapy directed against the overly exuberant immune response can be treated prior to ICU admission or intubation,” Cron said.
Several tests can be used to screen patients for cytokine storm syndrome. One of these is a serum ferritin test, which Cron says is “cheap, readily available, and quick.”
As for reducing the flood of cytokines in the body, many anti-inflammatory medications are being
Corticosteroids are one possibility. They reduce inflammation throughout the body. But they also have unwanted side effects, including increasing the risk of other infections.
More focused anti-inflammatory drugs are also being studied, including sarilumab, anakinra, emapalumab, and tocilizumab.
Tocilizumab targets a cytokine called IL-6, which is thought to be a
Anti-inflammatory drug may slow cytokine storm
The Food and Drug Administration (FDA) has also given the green light to clinical trials of compounds that were still being studied for use in other conditions.
One of those is a compound called CM4620-IE, which was developed by San Diego–based company CalciMedica for treating acute pancreatitis.
“The lung injury in acute pancreatitis is caused by the cytokine storm, which is the same thing that’s happening in COVID-19,” said Dr. Sudarshan Hebbar, CalciMedica’s chief medical officer.
By the time the pandemic hit, CM4620-IE had already made it partway through the clinical trial process for acute pancreatitis.
Dr. Charles A. Bruen, a critical care medicine physician and an investigator overseeing the CM4620-IE trial at Regions Hospital in St. Paul, Minnesota, says the initial results of those studies were promising, especially the effect of the drug on the lungs.
“We noticed in patients with acute pancreatitis who were also developing ARDS that their hypoxemia was getting better, that they were spending less time on the ventilator, and that they were leaving the hospital earlier,” he said.
Hebbar says in those patients, the cytokine level decreased rapidly, within 24 hours.
“We also showed that once we stopped the infusion of the drug, the immune system remained settled down,” he said, “but patients weren’t overly immunocompromised.”
The phase II clinical trial for CM4620-IE in COVID-19 patients is already underway. The drug will be given to patients with very early ARDS, before they need mechanical ventilation.
Hebbar says the company is rapidly increasing the number of clinical sites they’re working with and hopes to have results from this trial within 1 to 2 months.
After that, a phase III clinical trial with more patients will be needed.
While anti-inflammatory drugs slow the production of cytokines, technology also exists that can filter cytokines out of a patient’s blood.
The FDA issued an
Cron says plasmapheresis, or filtering plasma from the blood cells, has already been used to remove inflammatory cytokines in other cytokine storm syndromes.
“[So this process] may also prove beneficial in subsets of COVID-19 patients with features of cytokine storm syndrome,” he said.
Source: Read Full Article