Homozygous familial hypercholesterolaemia is often diagnosed late and is under-treated, causing hotspots of cardiovascular disease risk worldwide.
According to a new study in The Lancet, carried out by an international research collaboration including Imperial College London scientists, people with homozygous familial hypercholesterolaemia (HoFH) in low- and middle-income countries were less likely to receive the treatments they needed, compared with people in high-income countries.
As a result, only 3 percent of people in low- and middle-income countries had safe cholesterol levels (compared with 21 percent in high-income countries) and they had cardiovascular events, such as heart attacks and strokes, on average more than a decade earlier than people from high-income countries (at 25 years old, compared to 37 years old).
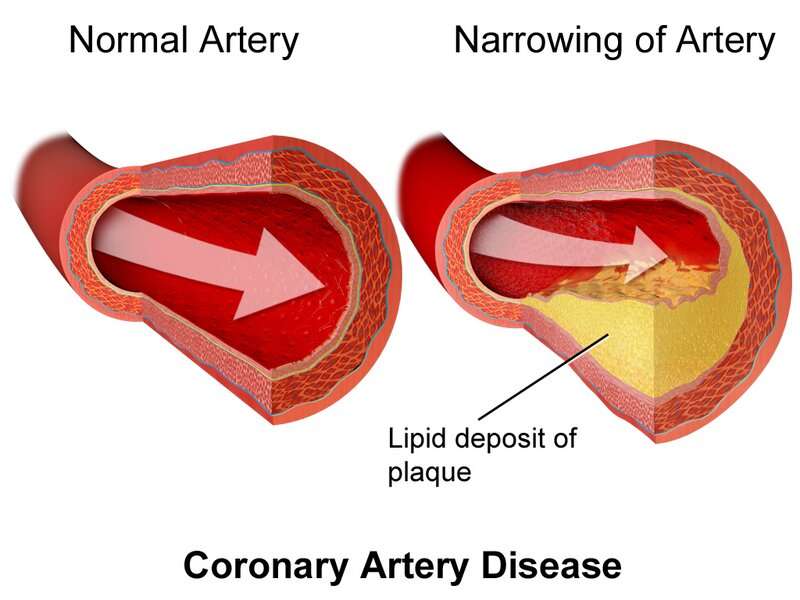
Study author Professor Kausik Ray, from Imperial’s School of Public Health, said: “HoFH affects around one in every 300,000 people and causes very high levels of low-density lipoprotein cholesterol—also known as LDL cholesterol—from birth.
“As this cholesterol is damaging, spotting cases early and ensuring they receive cholesterol-lowering therapy is essential to reduce the cardiovascular risk associated with the condition.”
The study is part of the Homozygous Familial Hypercholesterolaemia International Clinical Collaboration registry—the first registry of its kind, which is funded in part by the European Atherosclerosis Society—and was set up to learn about the characteristics and care of HoFH patients globally. Current care guidelines for HoFH are mostly based on small studies in high-income countries.
The new study included 751 people from 38 countries, including 18 low- and middle-income countries.
It found that almost one in 10 people (9 percent) had signs of cardiovascular disease or narrowing of the main heart valve when diagnosed with HoFH.
Only 534 people in the study had information on their treatment available. While statin use was similar in low- and middle-income countries and high-income countries (around 90 percent of people received them), there were stark differences in other treatments. For example, 73 percent of people in high-income countries received the cholesterol-lowering drug ezetimibe, compared with 54 percent in low- and middle-income countries.
Although people in low- and middle-income countries were diagnosed with HoFH around six years earlier than those in high-income countries, fewer people received additional cholesterol-lowering treatment combinations (24 percent vs 66 percent of people). As a result, people from low- and middle-income countries typically had higher LDL cholesterol levels (9 mmol/L vs 4 mmol/L, respectively, for people on lipid-lowering treatment).
Treatment re-evaluation needed
The researchers say that greater use of more potent novel cholesterol-lowering therapies in conjunction with statins and ezetimibe could reduce people’s risk of cardiovascular disease. They call for a re-evaluation of how the condition is treated and for better screening for it.
Professor Ray said: “With the greatest global burden for HoFH residing in less affluent regions of the world, a critical reappraisal of healthcare policy and funding is required at a global level to improve health outcomes for all patients with HoFH.
Source: Read Full Article