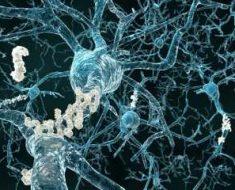
New research published in The Lancet Neurology journal suggests that frailty makes older adults more susceptible to Alzheimer’s dementia, and moderates the effects of dementia-related brain changes on dementia symptoms. The findings suggest that frailty should be considered in clinical care and management of Alzheimer’s dementia.
The study found that older adults (59 years and older) with higher levels of frailty were more likely to have both Alzheimer’s disease-related brain changes and symptoms of dementia, whilst others with substantial brain changes, but who were not frail, showed fewer clinical symptoms.
“By reducing an individual’s physiological reserve, frailty could trigger the clinical expression of dementia when it might remain asymptomatic in someone who is not frail,” explains Professor Kenneth Rockwood from Nova Scotia Health Authority and Dalhousie University, Canada, who led the study. “This indicates that a ‘frail brain’ might be more susceptible to neurological problems like dementia as it is less able to cope with the pathological burden.”
“This is an enormous step in the right direction for Alzheimer’s research. Our findings suggest that the expression of dementia symptoms results from several causes, and Alzheimer’s disease-related brain changes are likely to be only one factor in a whole cascade of events that lead to clinical symptoms. Understanding how individual risk factors work together to give rise to late-life dementia is likely to offer a new way to develop targeted treatment options.”
The findings support the idea that late-life dementia (and particularly Alzheimer’s disease) is a complex phenomenon rather than a single disease entity marked by genetic risk or single protein abnormalities in the brain. However, the authors caution that this study is a cross-sectional comparison of pathology data from a single database that only includes adults living in Illinois, USA.
Previous research has shown that some people with Alzheimer’s disease-related brain changes (eg, amyloid deposition) can have few characteristic symptoms of the disease (cognitive and functional decline), whereas others with few brain changes may have symptoms. These discrepancies suggest that some hidden factors might affect the relationship between Alzheimer’s disease-related brain changes and Alzheimer’s dementia.
Most people who develop Alzheimer’s dementia are older than 65 years and have several other health problems. Frailty — a condition linked with reduced physiological reserve and increased vulnerability to other ailments — is associated with age and higher rates of cognitive deficit and dementia, but little research has explored how these conditions might be related.
In this study, researchers used modelling to assess relationships between frailty, Alzheimer’s disease-related brain changes, and Alzheimer’s dementia among 456 participants of the Rush Memory and Ageing Project (MAP) who had either no dementia or Alzheimer’s dementia, and who subsequently died and underwent brain autopsy. MAP is a longitudinal clinical-pathological study of older adults living in Illinois, USA, which began in 1997.
Every year participants received neuropsychological and clinical evaluations, which included detailed cognitive testing and neurological examinations. Clinical diagnosis of Alzheimer’s dementia was based on clinician consensus, with just over half (53%; 242) the participants given a diagnosis of possible or probable Alzheimer’s dementia at their last clinical assessment. Brain plaques and tangles were measured after death to quantify Alzheimer’s disease-related changes. The researchers also developed a frailty index using a combination of 41 components of health status (eg, fatigue, joint and heart problems, osteoporosis, mobility, meal preparation) obtained at each clinical evaluation.
Overall, 35 participants (8%) had substantial Alzheimer’s disease-related brain changes without having been diagnosed with dementia, and 50 (11%) had Alzheimer’s dementia but had little disease-related brain changes (table 2).
The analysis revealed that frailty and Alzheimer’s disease-related brain changes independently contribute to dementia status, after adjusting for age, sex, and education.
The researchers also found a significant association between frailty and Alzheimer’s disease-related brain changes after excluding activities of daily living from the frailty index and adjusting for other risk factors such as stroke, heart failure, high blood pressure, and diabetes.
“While frailty is likely to reduce the threshold for Alzheimer’s disease-related brain changes to cause cognitive decline, it probably also contributes to other mechanisms in the body that give rise to dementia, weakening the direct link between Alzheimer’s disease-related brain changes and dementia,” says Rockwood.
“While more research is needed, given that frailty is potentially reversible, it is possible that helping people to maintain function and independence in later life could reduce both dementia risk and the severity of debilitating symptoms common in this disease.”
The authors say that future studies should examine longitudinal relationships between frailty, cognition, and biomarkers of Alzheimer’s dementia to establish causation. They also note several limitations, including that a single definition of frailty has not been well established — some definitions are more biological, others are more physical, whilst some combine physical, biological, psychological, and social risk factors. They also note that frailty measurements were taken close to death and might reflect terminal decline, which could result in the relationship between Alzheimer’s disease-related brain changes and dementia status among people with high levels of frailty being overestimated.
Writing in a linked Comment, Dr Francesco Panza from the University of Bari Aldo Moro, Italy, discusses how understanding frailty could help predict and prevent dementia. He concludes: “In light of current knowledge on the cognitive frailty phenotype, secondary preventive strategies for cognitive impairment and physical frailty can be suggested. For instance, individualised multidomain interventions can target physical, nutritional, cognitive, and psychological domains that might delay the progression to overt dementia and secondary occurrence of adverse health-related outcomes, such as disability, hospitalisation, and mortality.”
Source: Read Full Article