A new study has identified 228 clinical practices in Canada that are used inappropriately, with underuse being more common than overuse. This list includes diagnostic and therapeutic practices such as blood tests and radiography. Published in CMAJ (Canadian Medical Association Journal), the research can help health care professionals, organizations and governments improve patient care and health outcomes.
“The dominant finding from our review is that there are large gaps between the care people should receive and the care they do receive,” writes lead author Dr. Janet Squires, professor of nursing at the University of Ottawa and a senior scientist at The Ottawa Hospital, and coauthors. “We found that, on average, 30.0% of the care received by people in Canada as assessed in the included research papers using the Institute of Medicine’s definitions of underuse and overuse, was deemed inappropriate.”
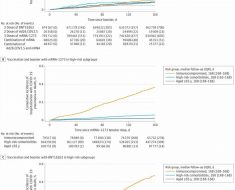
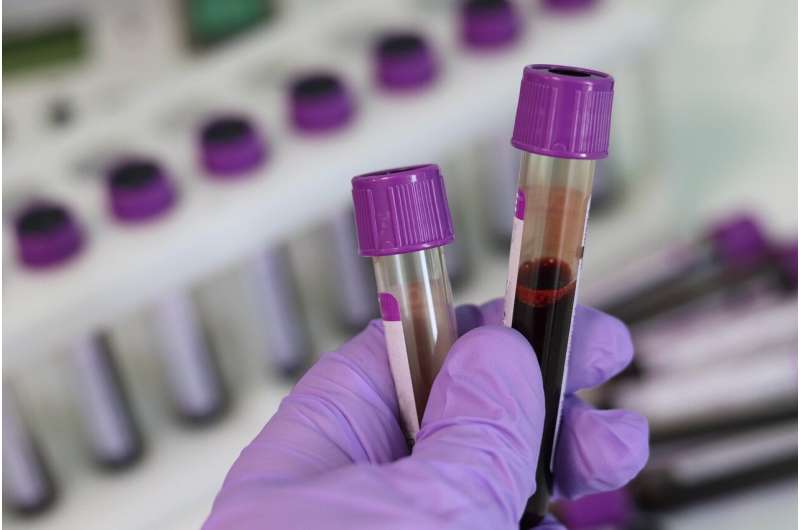
Researchers included 174 studies that evaluated whether clinical practices in Canada were meeting evidence-based guidelines. Together, these studies included 228 clinical practices and evaluated more than 28.9 million patients between 2007 and 2021. The researchers found inappropriate care in 30% of cases, with a median score of 44% for underuse and a median of 14% for overuse in diagnostics and therapeutics. Certain diagnostics were underused, such as glycated hemoglobin tests, lipid panel blood tests and diabetic eye exams. The most frequently overused diagnostics were the blood test for thyroid-stimulating hormone, chest radiographs and Pap tests.
Inappropriate care can lead to harm from the use or lack of use of a therapy or diagnostic procedure, contribute to negative patient experiences, and lead to poor health outcomes and inefficient use of scarce health care resources.
“We found that many clinical practices received by people in Canada are inappropriate; whether that practice is diagnostic or therapeutic, it frequently does not meet recommended standards,” the authors write.
They suggest that provincial and territorial governments, as well as quality improvement organizations, can use these findings to improve health care quality and conduct additional research. Clinicians can reference the list of clinical practices, especially the top 42 most-studied practices, to identify priorities for change.
In a related commentary, Dr. Kaveh Shojania, a general internist at Sunnybrook Health Sciences Centre, suggests that refocusing priorities on social determinants of health like housing, education, air and water quality, early childhood development and more could have greater impact than narrower system changes. This perspective is especially important, given the massive challenges facing the health system from the COVID-19 pandemic, the opioid epidemic and other threats.
Source: Read Full Article