After 100 years of insulin therapy, teplizumab, an immunotherapy for early-stage type 1 diabetes, has been approved for the first time in the United States and has been shown to delay the manifestation of clinical diabetes by 3 years on average. As a prerequisite for the use of the anti-CD3 antibody teplizumab, patients must undergo a general screening for type 1 diabetes. Whether this prerequisite makes sense was the subject of hot debate among experts at the Diabetes Congress in Berlin.
Anette-Gabriele Ziegler, MD, PhD, director of the Institute for Diabetes Research in Helmholtz Munich, argued that voluntary screening for type 1 diabetes should be included in standard care. “The first immunotherapy that delays type 1 diabetes has been approved in the US for early stage 2. And this early stage can only be identified through prior screening, since no symptoms have manifested by this stage,” she said. This is the only way in which as many people as possible, particularly children, will benefit from the disease-delaying therapy, she added.
Two Autoantibodies
One biomarker for the early diagnosis of type 1 diabetes is evidence of at least two positive islet cell antibodies. In one study of more than 13,000 children who were observed for 20 years, the specificity of these antibodies was 100%. “Every single child with a positive autoantibody test developed type 1 diabetes later on in their life,” Ziegler said. “Based on the results of this study, the early stages of type 1 diabetes were added to multiple guidelines.”
The early stage of type 1 diabetes is divided into the following three phases, depending on autoantibody detection and the level of glucose metabolism:
-
Early stage 1: Two or more islet autoantibodies and normoglycemia
-
Early stage 2: Two or more islet autoantibodies and dysglycemia
-
Early stage 3: Symptoms, hyperglycemia, insulin therapy
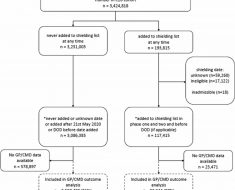
The aim of the ongoing FR1DA study is to ascertain whether the general population could also be screened for type 1 diabetes using this autoantibody. “Since 2015, children of kindergarten and school age have undergone screening, and to date, more than 170,000 have been tested,” said Ziegler. “At least two autoantibodies were detected in 0.3% of those screened.”
Education and Care
The families of the children in whom early-stage type 1 diabetes was diagnosed were invited to take an oral glucose tolerance test (OGTT), to undergo measurement of A1c, and to take part in training and monitoring. “Education and competent, ongoing care are crucial for the efficacy of the screening,” Ziegler emphasized.
The OGTT revealed that 85% of the FR1DA children were still in early stage 1, another 11% were in early stage 2, and the remaining 4% were in early stage 3.
“Unfortunately, the 4% could no longer benefit from teplizumab, since the medication is not approved for manifest diabetes,” said Ziegler. “However, the 11% could receive teplizumab immediately, and then later on, the 85%, when they developed stage 2. Therefore, further observation of the children is also important.”
The speed at which the disease progresses from early stage 1 to early stage 2 can be stratified using IA2 antibodies, the 90-minute OGTT glucose value, and the A1c value. With regard to progression to clinical type 1 diabetes (stage 3), it was observed that the progression risk for the FR1DA children was similar to that of international birth cohorts with increased genetic risk. “Of course, there is still no 20-year follow-up like for BABYDIAB, DIPP, and DAISY, but as of yet, the progression rate is practically identical,” said Ziegler.
Dubious Benefits?
The advantages of screening for type 1 diabetes would not be limited to potential access to preventive therapies and a smooth transition to insulin therapy at the correct point in time, according to Ziegler. Participation in the FR1DA study dramatically reduced the risk of diabetic ketoacidosis (DKA). Between 2015 and 2023, the overall rate of ketoacidosis associated with the manifestation of clinical type 1 diabetes was 4.3%. In contrast, the general DKA rate in Germany has remained largely unchanged for the last two decades at between 20% and 25%.
In addition, the FR1DA children exhibited better beta cell function and better metabolic function at clinical diagnosis of type 1 diabetes. This finding was observed in a comparison with children with a spontaneous diabetes diagnosis from the DiMelli study. “It is important that there is a lot of data that shows how, in the long term, this is associated with a better morbidity and mortality,” said Ziegler.
Despite the impressive data from the FR1DA study, not all diabetes experts are convinced that a general screening for type 1 diabetes would be beneficial. Beate Karges, MD, PhD, of the Clinic for Pediatric and Adolescent Medicine of the Bethlehem Hospital Stolberg and of the Endocrinology and Diabetology Department at the University Hospital Aachen, in Germany, stressed, “Screening makes sense if the disease is curable in the preclinical phase or if there is a significantly better prognosis in the event of early diagnosis and treatment.”
Severe Side Effects
Even with an early-stage diagnosis, curing type 1 diabetes is impossible. The new anti-CD3 antibody teplizumab merely delays the manifestation of symptoms for 3 years. However, this delay has its price. The summary of product characteristics for teplizumab contains warnings of severe lymphopenia lasting many weeks, cytokine release syndrome, severe infections, and hypersensitivity reactions. Furthermore, vaccinations may not be administered during teplizumab treatment and therefore must be completed in advance.
“Preventing type 1 diabetes is still not possible, we can only delay it, and the long-term efficacy and safety of this immunotherapy are not clear,” said Karges. She added that a significant reduction in the DKA rate — as observed in the FR1DA study — may be possible even without screening. This possibility was demonstrated by a model project in Stuttgart, Germany, in which the DKA rate was significantly reduced through education alone.
Education Reduces Ketoacidosis
“The families were given information about the early signs of type 1 diabetes during the education investigation. Through this [education], a reduction in the ketoacidosis rate from 28% to 16% was achieved,” said Karges. It is also known from studies of familial type 1 diabetes that secondary sufferers in the family only exhibit a DKA rate of 7%. “Through education within the family and awareness campaigns, the DKA rate can be reduced by 40% to 65%,” said Karges.
Karges also doubts whether starting insulin therapy earlier “at the correct point in time” elicits long-term advantages. Secondary sufferers with familial type 1 diabetes have better A1c values in the first few years after diagnosis. “But as they progress beyond 2, towards 10 years, the difference in HbA1c values diminishes,” said Karges.
Whether the patient has DKA at type 1 diabetes diagnosis also seems to make little difference in the long term. “There is also no difference in the HbA1c value in the 2 to 10 years after diagnosis,” said Karges. “Glycemic control is not permanently improved in the event that treatment is started early,” she concluded.
“Type 1 diabetes can be delayed with an immune intervention, but to do so, we must also accept possible severe side effects in an otherwise healthy child,” she said. On the other hand, type 1 diabetes can be treated well. “With pumps and continuous glucose monitoring, insulin therapy in children and adolescents has become significantly safer and more effective,” she said.
New Therapeutic Options
Whether the voluntary screening for type 1 diabetes eventually finds its way into standard care depends on the further development of preventive medications. Ziegler stressed that future preventive therapy does not need to be limited to the anti-CD3 antibody teplizumab.
For example, strategies such as high-dose oral insulin therapy are being investigated. Verapamil, which is used to treat hypertension, is also promising, since with it, beta cells were retained in early stage 3, and it improved their function. The fusion protein abatacept fell short of statistical significance in a recently published study. For Ziegler, one thing remains true. “The therapy of type 1 diabetes is about to undergo a renaissance.”
This article was translated from the Medscape German Edition.
Source: Read Full Article