NEW YORK (Reuters Health) – Researchers have developed an online tool to help clinicians predict which COVID-19 patients admitted to the hospital are likely to progress to severe disease.
The tool, Severe COVID-19 Adaptive Risk Predictor (SCARP), is available at https://bit.ly/3btwEWS.
“Clinicians need to have measurements of vital signs and a few basic labs to maximize use of the tool,” Dr. Matthew Robinson of Johns Hopkins University School of Medicine in Baltimore told Reuters Health by email. “It is designed to begin giving predictions with input of only two variables – pulse oximetry and amount of supplemental oxygen being used – but then delivers increasingly accurate predictions as more variables are entered.”
“We included ‘Adaptive’ in the name,” he explained, “because the tool sequentially asks clinicians for the next most important variable needed to improve the accuracy of the prediction, which is tailored to the information already inputted.”
Recent studies have found that traditional risk scoring tools may be unreliable in COVID-19 patients. Last month, for example, a separate research team reported in JAMA that for determining the need for mechanical ventilation in patients with COVID-19 pneumonia, the accuracy of the Sequential Organ Failure Assessment (SOFA) score “was poor and significantly inferior to simply using age.” (http://bit.ly/3aJQMnb)
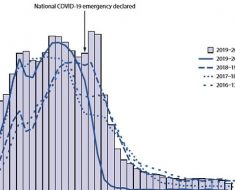
As reported in Annals of Internal Medicine, the SCARP tool was developed based on COVID-19 registry data collected between March 5 and December 4, 2020, including demographic characteristics, hospital admission source, comorbid conditions, time-varying vital signs, laboratory measurements, and clinical severity. Healthcare workers recording the data were blinded to subsequent patient outcomes.
The primary outcome was progression to severe illness or death, according to the WHO COVID-19 score of 6 or greater, including patients who died or received respiratory support.
Data from 3,163 patients hospitalized with moderate COVID-19 were included in the analysis. The median age was 61; 51% were men; 31%, non-Hispanic White; 36%, Black; 23%, Hispanic; 5% Asian and 5% unknown.
Of these, 228 (7%) became severely ill or died in the next four hours; an additional 355 (11%) became severely ill or died in the next week.
The area under the curve for one-day predictions to severe illness or death was 0.89 during the first or second week of hospitalization.
The AUC for one-week predictions was 0.83 during the first week and 0.87 during the second week.
Model calibration, assessed by risk decile, showed that the one-day and one-week risk predictions were well calibrated.
One limitation is that the tool is based on data from a single healthcare system. “We will be evaluating and refining our tool using larger national databases,” Dr. Robinson said. “We intend to expand our focus to predict who is well enough to be safely discharged home and who is at highest risk of death among patients who are already severely ill. We also hope to apply these methods to predict the outcomes of other infectious diseases.”
Dr. Jess Mandel, Chief, Division of Pulmonary, Critical Care, and Sleep Medicine and Vice-Chair for Education, Department of Internal Medicine at UC San Diego School of Medicine in La Jolla, commented by email to Reuters Health, “It is an interesting first step, but is not ready for implementation. It will need to be validated in patient cohorts separate from the ones from which it was derived and in multiple diverse settings before its use could be recommended.”
“A lot of the most powerful predictive components are already pretty apparent to people who take care of a lot of COVID-19 patients,” he noted, “so the incremental benefit to experienced clinicians remains to be seen.”
“Defining better clinical prediction rules could be helpful in terms of allocating healthcare resources and in reassuring patients who are low risk,” he added. “However, it is a challenge in a new disease like COVID-19, where it is a bit of a moving target. As more patients become vaccinated, their clinical course, if infected, will be very different from the patients from which the risk predictor was derived and it likely won’t be valid. Likewise, as additional treatments become available, it becomes less relevant.”
SOURCE: https://bit.ly/3btXmyo Annals of Internal Medicine, online March 2, 2021.
Source: Read Full Article