Children with obesity, who have recently lost weight, are more likely to show hunger-related activity in their brains after a meal, according to research presented today at the 60th Annual European Society for Paediatric Endocrinology Meeting. This brain activity, reflecting that they were unsatisfied by their meal, happens even though their gut hormone levels have changed, as expected, to reduce hunger and indicate fullness. This disconnect between food satisfaction in their brain versus their digestive system may underlie why many people regain weight, particularly after a strict diet. Understanding and addressing this persistence of hunger-promoting brain activity could lead to better and more sustainable treatments for obesity in children and adults.
Obesity is a growing worldwide health crisis with an estimated 124 million children affected globally. Obesity increases the risk of many other health problems including type 2 diabetes, heart disease and cancer. Obesity in children is often managed through family-based behavioral therapy involving regular outpatient sessions that focus on dietary and physical activity education. In the USA, the gold standard for such programmes is a minimum of 26 contact hours over a 6 month period, however, many children regain weight soon after programme completion. It is poorly understood why the success rate is so low. Appetite and metabolism, and therefore weight gain, is regulated by activity in both the brain and the digestive system. Understanding how these processes are affected by weight loss may help us better understand the mechanisms that predispose children to rebound weight gain.
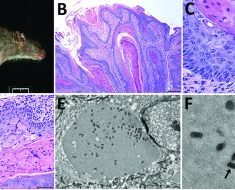
In this study, Professor Roth and colleagues at Seattle Children's Hospital in the USA, compared brain appetite regulation activity with gut hormone responses in children with obesity before and after a 24-week weight loss programme. Using functional MRI, they assessed activation patterns in appetite-regulating brain areas in response to high- vs. low-calorie images, after a meal. Gut hormone levels were also assessed before and after meals, at the beginning and end of the programme. At the end of the programme, children still showed high levels of activation in brain areas related to appetite, after a meal, in response to food images, indicating that they were hungry. However, their levels of appetite-regulating gut hormones indicated fullness and satiety. Strikingly, the children who lost the most weight, showed the strongest activation in their brains to food cues after a meal, at the end of the programme.
Our results imply that during weight loss intervention, your body acts to conserve fat through maintaining hunger responses in the brain, and that this needs to be addressed, perhaps through drug treatment, for successful and sustained weight loss in children with obesity."
Professor Roth, Seattle Children's Hospital, USA
Although Professor Roth cautions, "These findings are from a small group of children tested only at the start and end of the intervention programme, so larger and more detailed studies would be needed to confirm this central effect. It would also be useful to investigate how long the disconnect between central and local appetite regulation persists after maintained weight loss, to guide intervention plans."
Professor Roth suggests, "For more successful treatment of obesity in children, we should avoid interventions that lead to fast body weight reductions and instead aim for more gradual and consistent lifestyle changes, over years rather than months, which will lead to sustained and long-term improvements in weight loss and health."
European Society for Paediatric Endocrinology
Posted in: Child Health News | Medical Research News
Tags: Adiponectin, Brain, Cancer, Children, Diabetes, Diet, Digestive System, Education, Endocrinology, Food, Functional MRI, Ghrelin, Glucagon, Glucagon-like Peptide-1, Heart, Heart Disease, Hormone, Hospital, Leptin, Medicine, Metabolism, Neuroimaging, Obesity, Physical Activity, Research, Type 2 Diabetes, Weight Loss
Source: Read Full Article