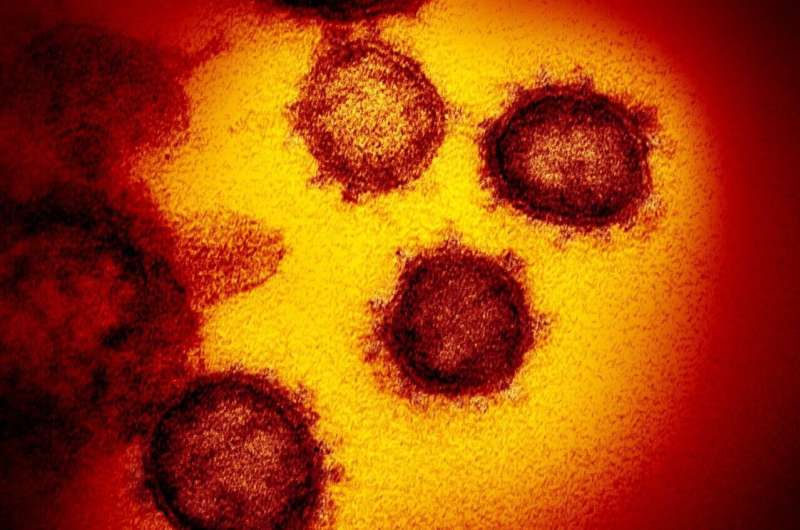
COVID-19 outbreaks in French nursing homes almost certainly started in staff—and none of measures put in place stopped the virus from taking hold, new research being presented at the European Congress of Clinical Microbiology & Infectious Diseases (ECCMID), held online this year, shows.
Residents of long-term care facilities represent a small fraction of the general population but account for a disproportionate number of SARS-CoV-2-related deaths in many countries.
In France, 5,203 outbreaks (of 1 case or more) were reported in nursing homes during the first wave of COVID-19. In the Auvergne-Rhône-Alpes region, there were 651 outbreaks, 3,885 residents had confirmed COVID-19 infection and 1,772 (46%) subsequently died.
Little is known, however, about how the COVID-19 virus enters nursing homes nor how it spreads in this complex environment.
Emilie Piet, of the Centre Hospitalier Annecy Geneva, Epagny Metz-Tessy, France and colleagues, carried out a cross-sectional survey in nursing homes in the French Alps from March 1 to May 31 May 2020.
The survey covered cases of COVID-19 among residents and staff during the first lockdown, as well as the staffing during the pandemic, including staffing levels and the use of interim carers.
It also asked about the nursing homes’ characteristics (e.g. number of residents, whether these were private or public facilities, if they cared for dementia patients) and hygiene measures implemented (these included wearing face masks, confining residents to their rooms, use of alcohol-based hand sanitiser and bans on visits).
Seventy four (33%) of 225 nursing homes completed the survey. A total of 22 homes, with 1,795 residents in total, had an outbreak of COVID-19—defined as at least three cases. (See table 1 of abstract).
In the homes with outbreaks, 26% (473/1,795) of the residents had a confirmed or probable case of COVID-19; 19% (341/1,795) of residents were hospitalized and 253 (14%) died of any cause.
In contrast, 0.2% (9/4,096 residents) of residents in the outbreak-free homes had confirmed or probable COVID-19, 6% (247/4,096) were hospitalized and 6% (250/4,096) died of any cause during the period studied.
A total of 19% (250/1,348) of staff in the homes with outbreaks had confirmed or probable cases of COVID-19, compared to 1.4% (46/3,304) in the outbreak-free homes.
The results revealed a strong link between cases in staff and cases in residents.
Further analysis showed that cases of COVID-19 in staff were the only predictor of an outbreak among residents.
In other words, none of the nursing homes’ characteristics seemed to have any effect and nor did any of the hygiene measures. However, the homes all employed similar hygiene measures, making it difficult to tease apart their effect, says Dr. Piet.
She adds: “This study shows that when strict hygiene measures are implemented in nursing homes, factors such as the number of beds, the ratio of staff to residents and the use of temporary staff do not influence outbreaks.
Source: Read Full Article