Pneumococcal conjugate vaccines (PCVs) have been highly effective in reducing pneumonia and other invasive infections caused by Streptococcus pneumoniae bacteria. But rates of meningitis have shown little change, as pneumococcal strains not targeted by PCVs emerge as more important causes of meningitis, reports a paper in The Pediatric Infectious Disease Journal, the official journal of The European Society for Paediatric Infectious Diseases.
Reshmi Mukerji, MPH, and David E. Briles, Ph.D., of University of Alabama at Birmingham analyze evidence on how pneumococcal meningitis has changed since the introduction of PCVs. To make progress in reducing rates of meningitis worldwide, the researchers believe that new vaccines targeting all pneumococcal strains colonizing the nose and throat, irrespective of capsular type, will be needed.
PCV Vaccines Linked to Emergence of New Strains Causing Meningitis
The PCV7 and PCV13 vaccines—targeting seven and thirteen strains of pneumococcal bacteria, respectively—have been highly effective in reducing rates of invasive pneumococcal disease, including pneumonia and bloodstream infection or sepsis. But despite the use of PCVs, pneumococcal bacteria remain the leading cause of meningitis in children. Worldwide, meningitis rates of up to 13 cases per 100,000 children have been reported.
Bacterial meningitis is infection of the brain and spinal cord membranes: it is difficult to treat, often fatal, and causes lasting complications in survivors. Recent studies have shown that child and adult pneumococcal meningitis rates have been stable or increased, largely due to bacterial strains not targeted by PCVs.
“Widespread use of vaccines resulted in the emergence of a broad diversity of replacement non-PCV type strains,” Ms. Mukerji and Dr. Briles write. Although this serotype replacement has occurred worldwide, evidence suggests that rates are highest in Europe and North America. These non-vaccine-type strains cause meningitis at least as severe as the types targeted by PCV7 and PCV13.
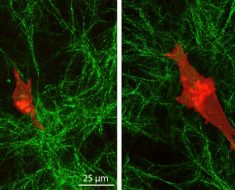
Many pneumococci covered by PCV 13 form capsules that shield them from the body’s immune system in the lung and blood. However, the replacement strains seldom cause sepsis—suggesting that their non-PCV capsules don’t allow them to survive well in the bloodstream. The pneumococci with non-PCV type capsules may be traveling to the brain directly from the nose, throat and ear, through the olfactory and auditory nerves, rather than through the bloodstream.
This could occur when the nose and throat are colonized by pneumococci of non-PCV capsular types, which have largely replaced the bacteria targeted by current PCVs. To prevent such cases of meningitis, new vaccines will need to be developed to prevent or greatly reduce colonization with these capsular, non-vaccine-type bacteria.
The problem is that there are more than 98 different capsular types—it would be difficult or impossible to target them all in a single vaccine. The most promising alternative might be vaccines directed at specific proteins involved in pneumococcal capsule formation and colonization. The authors outline an approach where this strategy could first be tested in small-scale studies, before larger studies to confirm its effectiveness in preventing meningitis.
Source: Read Full Article