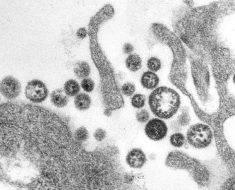
A unique collection of tissue samples donated by people with chronic myeloid leukemia was the driving force behind the discovery of a potentially major new treatment approach for drug-resistant leukemia. As published this week in the Proceedings of the National Academy of Sciences, researchers report how a laboratory study of a specially engineered formulation of gas, composed of charged and highly reactive molecules, called “cold atmospheric plasma,” or CAP, was highly effective in targeting drug-resistant leukemia cells while protecting nearby healthy cells.
There are many types of leukemias that arise in bone marrow cells. While research has led to major improvements in the survival of adult and child leukemia patients, some leukemias that were at one time responsive to treatment become resistant to the drugs used to target them. Therefore, scientists are working to improve treatment options for leukemia patients by understanding the characteristics of aggressive leukemias that are more likely to develop drug resistance.
The study was powered by a unique resource at Huntsman Cancer Institute (HCI) at the University of Utah (U of U) called the HCI Hematology Biobank. This resource provided patient-donated leukemia samples with the precise characteristics needed to conduct the study to determine how CAP blocks strategies leukemia cells use to survive.
Study co-first author Tony Pomicter, MS, leads the team that runs HCI’s Hematology Biobank. “Our entire team of study coordinators, specimen processors, database specialists, and healthcare providers spent many years collecting thousands of samples donated by thousands of patients at Huntsman Cancer Institute so we could have just the right diagnosis, cell type, cell count, treatment histories, and mutations for this study,” he said.
Pomicter credits the critical partnership between patients, doctors, and laboratory scientists in driving cancer research discoveries forward. In 2019 alone, more than 450 patients donated samples to HCI’s Hematology Biobank. Collected samples are tied to the patient’s medical record, providing a high degree of precision on the unique characteristics of the cells at the time of collection; for example, whether the sample is prior to treatment or after a relapse.
The HCI team was approached for samples from the Hematology Biobank by Michael Kong, Ph.D. and Hai-Lan Chen, Ph.D., the corresponding authors of the study and professors at Old Dominion University, Norfolk, Virginia. Kong, a biomedical engineer, and Chen, a molecular biologist, were working on understanding how CAP could be tailored to specifically target drug-resistant leukemia cells. Previous work demonstrated anticancer activity of CAP by containing or generating chemical and physical effectors. Kong and Chen noted that the biological effectors in certain CAP preparations can activate cancer cell survival and actually make the cells drug-resistant, so they knew that studies on cancer cells taken directly from patients would be key to understanding how to formulate CAP to instead prevent cancer cell survival and drug resistance.
Kong, Batten Endowed Chair in Bioelectrics at Old Dominion University, reflects how the journey to the discovery started in a different field. “In our work in developing CAP to overcoming drug-resistant
microbial pathogens, we noted that an excellent antimicrobial activity of CAP is centered on the cooperation of its many components,” he said. “We reasoned that potent anticancer activity may be achieved by engineering such cooperation of CAP’s many components at very low doses to kill cancer cells. To our surprise, the strategy of leveraging the cooperation of diverse, low-dose reactive oxygen species, ions and other effectors actually enables simultaneous blockade of three fundamental cancer cell resistance pathways, leading to a very high-rate of death in drug-resistant leukemia cells.”
Kong cites the central importance of the interdisciplinary cross-fertilization between gas plasma physicists, biomedical engineers, and molecular biologists as well as the catalyst of working with Huntsman Cancer Institute.
Chen, research associate professor in molecular biology, agrees. “Chronic myeloid leukemia is an exceptional model to test CAP since it is caused by a single molecular event and the mutations are well understood,” Chen said. “Efficacy data with chronic myeloid leukemia cells allowed us to establish a clear picture of the underlying mechanisms with little risk of ambiguity. We look forward to future collaborations with Huntsman Cancer Institute to take this work forward on leukemia and other cancers.”
Kong and Chen worked with the HCI team to identify the specific samples from the HCI Hematology Biobank for study. Using the detailed records the HCI team has developed for its biobank, they identified blood samples with the most difficult-to-treat mutation, as well as samples from healthy donors. These leukemia and healthy cells were cultured in the lab so the team could conduct experiments using different formulations of CAP. “It was critical to evaluate healthy cells alongside leukemia samples,” says Pomicter. “We always need to understand whether a novel agent is killing all cells, which means it is a toxin, or selectively killing cancer cells, which means it is potentially a drug.”
Source: Read Full Article