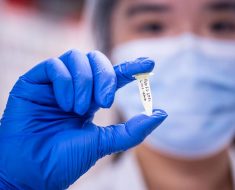
Fat pill which tricks the brain into thinking it is full is going to be tested on humans – and it could be available to take within five years
- The pill suppresses appetite by tricking the gut into feeling full with hormones
- Forty volunteers of varying high weights are needed for the study in London
- Researchers have high hopes it could reduce surgeries and type 2 diabetes
A ‘fat pill’ that could help millions beat the bulge could be available within five years, researchers believe.
The capsule works by suppressing the appetite, tricking a person into thinking they are full.
It has already been tested in the laboratory for over four years, but researchers are now beginning human trials.
Should it work, scientists claim it holds potential as a ‘major weapon’ for solving the global obesity crisis.

A ‘fat pill’ could be available within five years as researchers at Queen Mary University of London ask people to come forward for a trial
Forty volunteers aged 18-75 will be recruited by scientists at Queen Mary University of London.
Over 18 months, the participants will help to establish the correct dosage levels and manage any side effects that appear.
The first phase, involving 20 participants who are overweight, but not necessarily obese, will confirm if the pill does reduce appetite.
They must not have had bowel surgery, a bowel disorder or be taking medication for type 2 diabetes.
The second phase, a further six months, will test the efficacy on 20 participants who are obese or on the waiting list for a gastric bypass.
-

‘Jesus is a Malteser and Paddy is a fat, damp, squishy…
British mothers are being let down: Almost a QUARTER are…
A stranger’s silly prank on holiday left our poor boy in a…
Grandmother cannot remember the past 40 years after blacking…
Share this article
The capsule is packed with a mix of natural oils. Participants would take the pill before every meal.
It would send special food supplements directly to the lower bowel, bypassing the small intestine, causing the release of hormones such as insulin which suppress appetite.
Dr Madusha Peiris, from QMoL, said: ‘Getting the body to release hormones that make you feel full will reduce appetite and reduce food intake.
IS OBESITY IN YOUR GENES?
A study has found being thin is very much in your genes, so that many people can stay slender with no willpower required.
Scientists led by the University of Cambridge have identified a series of genes which may speed up someone’s metabolism or help them burn fat more quickly.
These genes were found in more than 1,600 thin but healthy people, including women around a size eight and men with a 35ins waist.
In almost two-thirds of these people, it is believed these genes make them less interested in food.
However the results also confirm what less slender people have long suspected.
In 40 per cent of the study group, thin people said they loved food and ate whatever they wanted without putting on weight.
Researchers now believe these people have particular genes of their own and are planning a separate study to see what happens in their bodies when they overeat.
It could lead to new drugs which mimic the effects of these ‘thinness’ genes and are used to help less lucky people keep the weight off.
‘It works in the same way as gastric bypass surgery but without the irreversible, expensive surgery which is often only available to obese patients.
‘The “fat pill” is just like swallowing a fish oil capsule. It’s a totally novel idea and we’re very excited to be proceeding to human trial.
‘We are hopeful that the treatment will be widely available in the next five years.’
Professor Ashley Blackshaw, from QMoL, said: ‘If the trials work, this could be a major weapon in tackling the obesity crisis and type 2 diabetes.
‘It could also cut the need for gastric bypass surgery which costs the NHS millions every year.’
Weight-loss surgery has increased 30-fold in the last decade, with more than 8,000 operations take place annually on the NHS, and many more through private clinics.
Also called bariatric surgery, it is used as a last resort to treat people who are dangerously overweight.
Privately the costs are £5,000-£8,000 for a gastric band, and up to £15,000 for gastric bypass surgery.
The human trials are being funded through the charity Bowel and Cancer Research with the support of the JP Moulton Charitable Foundation.
Deborah Gilbert, chief executive of Bowel and Cancer Research, said: ‘Being overweight is now recognised as a major risk factor for bowel cancer.’
Obesity is the second biggest preventable cause of cancer in the UK, according to Cancer Research UK.
More than one in 20 cases of cancer are caused by excess weight, associated with two of the most common cancers – bowel and breast cancer.
At the same time, obesity levels are increasing; millions of people in the UK are obese – around a quarter of adults and a fifth of children.
Source: Read Full Article