A significant concern after a person receives an organ transplant from a donor is antibody mediated rejection (AMR)—a process by which antibodies in the recipient can cause their immune systems to reject and damage the donor organ. This can lead to loss of the transplanted organ and even death in some cases.
It has been difficult to create human experimental models of rejection, and as a result researchers have had little opportunity to investigate therapies that might reduce the risk of this devastating complication and to elucidate new mechanisms. However, King’s College London researchers have today published a clinically relevant, reproducible, and translational model of AMR using human kidneys and warm machine perfusion technology, for what is believed to be the first time.
The study, published in eBioMedicine, was authored by post-doctoral researcher and transplant trainee Pankaj Chandak and senior authors Professors Anthony Dorling and Nizam Mamode, alongside colleagues in the School of Immunology & Microbial Sciences at King’s College London, Guy’s and St Thomas’s Trust NHS Foundation Trust and King’s Health Partners.
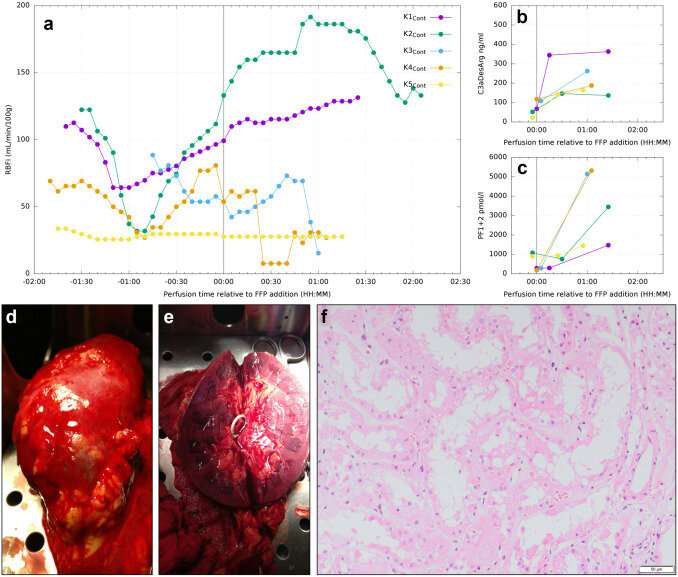
By connecting a human organ (offered for research purposes) to a bypass machine and circulating warm blood-based solutions through the organ (known as warm machine perfusion), then deliberately adding antibodies and complement and coagulation factors to the circuit, the researchers can artificially induce and simulate AMR. In so doing, they may be able to study transplant rejection mechanisms more closely, and hopefully gain greater insight into how this condition may be prevented.
Most notably, the model may allow researchers to investigate and test targeted organ-specific therapy. Strong immunosuppressors are often used to prevent donor organ rejection, but use of these drugs puts recipients at risk of other complications such as sepsis. Targeted organ-specific therapeutics, however, may allow doctors to treat only the intended organ, lessening the risks posed to the body.
“The development of an experimental human model of transplant rejection using warm machine perfusion may allow testing of targeted organ-specific therapy and to gain further mechanistic insight into this process. We may then also investigate repair and regeneration interventions in these rejected, injured organs. This could then hopefully be used to help real patients,” said Pankaj Chandak, lead author of the research.
In addition to improving treatment options for AMR in kidney transplant patients, the authors believe the insights gained from this model and its setup could also be transferable to other solid organ transplant types.
More information:
Pankaj Chandak et al, Modelling acute antibody-mediated rejection of human kidney transplants using ex-vivo warm machine perfusion, eBioMedicine (2022). DOI: 10.1016/j.ebiom.2022.104365
Journal information:
EBioMedicine
Source: Read Full Article





