Free influenza (flu) vaccines are now available for eligible groups, subject to local supply arrangements, with health authorities encouraging booking in from mid April.
For those who aren’t eligible for a free vaccine, flu shots are available now for a small fee (around A$25) from pharmacies and GPs (though you might also have to pay a consultation fee).
This year, you can get your flu shot on the same day as your COVID booster.
Not ‘just the flu’
Influenza is a disease of the respiratory tract. It can cause a runny nose, coughing, sneezing, sore throat, fever and chills, headache and body aches. It can cause vomiting and diarrhea, which is more common in children.
Influenza affects people of all ages and can cause severe illness and lead to hospitalization and death, particularly in young children, the elderly and those with underlying health conditions.
The number of cases and deaths in Australia each year fluctuates. In 2019, before the pandemic, 313,000 lab-confirmed cases and 953 deaths were reported. The 2019 case numbers were 2.7 times higher than the five-year average.
In the first two years of the pandemic, flu numbers plummeted due to prevention measures used to content COVID spread.
When do they start working? How long do they last?
Vaccines don’t cause disease in the person. Rather, they prompt the body’s immune system to respond, much as it would have on its first reaction to the actual virus.
Flu vaccines stimulate antibodies to develop in the body usually within two weeks following vaccination.
While flu vaccines offer the highest level of protection three for four months after vaccination, research suggests antibodies continue to protect against infection 8.5 months after vaccination and 11.8 months after natural infection.
So while antibodies decrease over time, they generally last longer than a typical influenza season.
Current recommendations are to get vaccinated from April, before the flu season, which generally occurs from June to September.
Why do we need a flu vax each year?
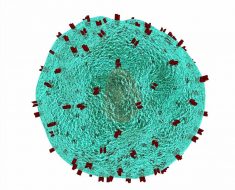
There are four types (or strains) of influenza viruses: A, B, C or D. Types A and B cause severe disease in humans, and each year the seasonal flu vaccine protects against two A and two B strains.
The four types are related to the presence of specific proteins on the surface of the virus. These surface proteins aren’t stable and often mutate, or change.
When the body encounters these changes, the immune system cannot be activated.
So although the person may have been vaccinated against or infected by a “old” version of the viral strain, the body won’t easily recognize and neutralize the new strain.
Due to these continuous changes, the World Health Organization reviews and updates its recommendations for the composition of the vaccine annually. It selects the viruses (mutated versions of the virus) most likely to circulate in the coming season.
The Australian Influenza Vaccine Committee uses this recommendation to determine the composition of influenza vaccines for use in Australia.
Our 2022 seasonal flu vaccine protects against:
- an A/Victoria/2570/2019 (H1N1)pdm09-like virus
- an A/Darwin/9/2021 (H3N2)-like virus
- a B/Austria/1359417/2021-like (B/Victoria lineage) virus
- a B/Phuket/3073/2013 (B/Yamagata lineage)-like virus.
However, some vaccines protect against three strains (trivalent, covering one B strain) rather than four (quadrivalent, covering two B strains).
While it’s generally better to get the four-strain vaccine, the success of the vaccine depends on whether it matches (and therefore protects against) the strain or strains dominating that season.
Who should get vaccinated?
Annual vaccination is the most important measure to prevent influenza and its complications.
Vaccination does more than just protect an individual: sufficient vaccination levels across the community can protect members of the community who would otherwise be left vulnerable.
The seasonal flu vaccine is recommended for all Australians aged six months and over.
It’s available for free to the population groups most as risk of severe disease from influenza:
- people aged 65 years or over
- children aged six months to under five years
- pregnant women at any stage of pregnancy
- Aboriginal and Torres Strait Islander people aged six months and over
- people aged six months or over who have medical conditions that mean they have a higher risk of getting serious disease.
For over-65s, adjuvanted influenza vaccines—which include an immune-stimulant to encourage a stronger immune response—are recommended over standard influenza vaccine.
How effective are vaccines?
Vaccine effectiveness varies depending on the outcome being measured, the age group affected (as vaccine effectiveness is generally lower in older people), and the match between vaccine and circulating influenza strains.
Estimates of flu vaccine effectiveness is 40–60% in the United States and 30–60% in Australia. This means 30–60% of those vaccinated are less likely to become seriously ill or die from influenza.
What about side effects?
Most influenza vaccines are safe in adults and children.
However, they can sometimes cause side effects. These include fever, muscle pain, vomiting, nausea, headache, irritability, injection site reaction and rash.
Source: Read Full Article