New research from the University of Minnesota’s Carlson School of Management illustrates that there is an association between the implementation of statewide stay-at-home orders and a reduction in the number of people hospitalized for COVID-19.
The research, published in JAMA, analyzed hospitalization rates before and after stay-at-home orders were issued in Colorado, Minnesota, Ohio and Virginia.
“What we found is that about 12 days after the stay-at-home order was implemented, the growth in hospitalizations began to deviate favorably from the initial, projected trajectory,” said Soumya Sen, associate professor in the Carlson School and the study’s lead author. “In all the states we examined, growth in the total number of patients being hospitalized due to COVID-19 symptoms appeared to slow down from the initial, exponential trend.”
The four states examined were the only states that met the study criteria:
- issuance of a statewide stay-at-home order;
- at least seven consecutive days of cumulative hospitalization data for COVID-19 patients (i.e., those currently hospitalized and those released) before the stay-at-home order was implemented; and
- at least 17 days of cumulative hospitalization data following the order date.
“Looking at real-time hospitalization data and how it responds to stay-at-home orders is critical for continuously designing and adjusting policies,” said Pinar Karaca-Mandic, professor and academic director of the Medical Industry Leadership Institute in the Carlson School, and study co-author. “As the number of COVID-19 cases fluctuate, states’ responses must balance containment efforts with health outcomes in mind.”
Using data collected from each state, the study authors calculated the projected growth in hospitalizations based on hospitalization information leading up to the stay-at-home order and compared it to the actual number of hospitalizations that occurred in each state.
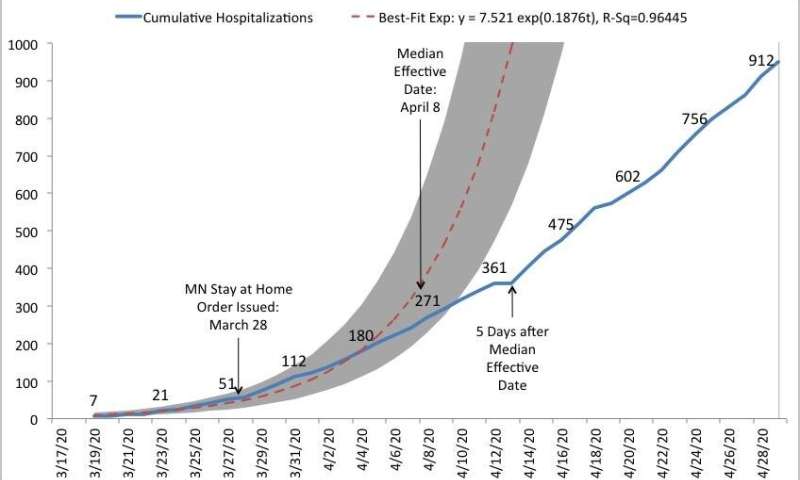
Prior to the issuance of the stay-at-home order and the 12-day incubation period immediately following it, the researchers found the best fit of the exponential growth curve—the dotted red line in each state’s graph—closely coincided with the actual number of increased hospitalizations in each state. However, following the 12-day incubation period—when the order would start to have an impact—the number of actual hospitalizations deviated from the projected curve to mark a slowdown.
In Minnesota, the 95% prediction band—shaded in gray—estimates how many total hospitalizations might have occurred if the initial growth trend continued in the absence of a stay-at-home order. By April 13, 2020, five days after the end of the incubation period, projected hospitalizations were 988 while the actual hospitalizations were 361.
Similar results were found in the other states at the five day mark:
- In Colorado, projected hospitalizations were 8,637; actual hospitalizations were 1,632.
- In Ohio, projected hospitalizations were 4,353; actual hospitalizations were 1,612.
- In Virginia, projected hospitalizations were 2,335; actual hospitalizations were 1,048.
A variety of additional factors may have contributed to the slowing hospitalization rate, including a declaration of national emergency; school closures; a growing, general awareness about social distancing; and good hand hygiene practices. However, some of these measures were already in place before the study’s designated period.
“The observation that hospitalizations decreased after the 12-day median incubation period following the issuance of the stay-at-home orders suggests that these orders are an important contributing factor to slowing down hospitalization rates,” said Sen.
“We are getting smarter about the effect of various interventions aimed at mitigating the spread of this virus, whether it’s masks or stay-at-home orders,” said Archelle Georgiou, chief health officer at Starkey Hearing Technologies and study co-author. “We hope these study results offer valuable insight to public policymakers; they need to understand the degree to which this intervention may be able to control the pandemic.”
Source: Read Full Article