Scientists led by Julia Sacher from Max Planck Institute for Human Cognitive and Brain Sciences and Osama Sabri from the Leipzig University Hospital have discovered in an elaborate patient study that the transport of the neurotransmitter serotonin in the brain increases in women with premenstrual dysphoric disorder (PMDD) shortly before menstruation. Their findings provide the basis for a more targeted therapy of this specific mood disorder, in which patients only have to take antidepressants for a few days.
PMS, or premenstrual syndrome, is now a familiar term to many—about 50% of all women experience these symptoms a few days before onset of their menstruation. The more severe form, called premenstrual dysphoric disorder (PMDD), affects eight percent of women of childbearing age and is associated with physical symptoms such as sleep disturbances or breast pain as well as psycho-emotional symptoms, including depression, loss of control, irritability, aggressiveness and concentration problems. As a result, many women with PMDD experience disruptions in their personal and professional lives.
It is assumed that PMDD in affected women is mainly caused by a hypersensitivity to the normal changes in the sex hormones estrogen and progesterone, as their concentrations fluctuate greatly in the second half of the cycle and after ovulation.
“We know that estrogen and progesterone have an influence on serotonin levels, which in turn directly affects mood. In patients with PMDD, the brain’s response to these changes in the cycle seems to be dysregulated,” explains study leader Julia Sacher. Together with her colleagues from the clinic of nuclear medicine at Leipzig University Hospital, she therefore took a closer look at the role of the neurotransmitter serotonin in the brains of PMDD patients.
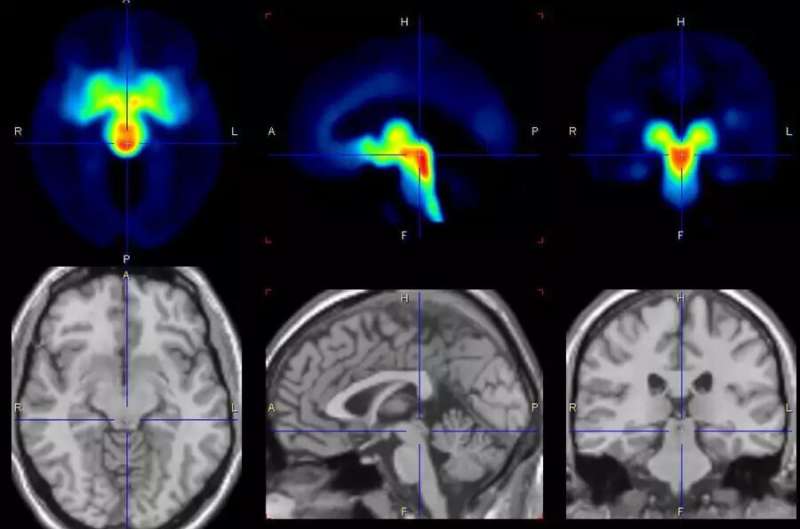
“We examined 30 female patients and 29 healthy study participants over several menstrual cycles and took images of the brain with positron emission tomography (PET) at different cycle times. We found that shortly before menstrual onset, the serotonin-transporter in the brain is increased and thus promotes a synaptic loss of this neurotransmitter, which can explain the affective symptoms in the affected women.
“This finding is surprising because it was previously thought that serotonin transporter density could not change in a short time span of two weeks—normally this is considered to be an individual trait with only minor changes over the period of 10 years is assumed.”
These short-term changes in serotonin transporter provide the evidence for a cycle-phase specific therapy of PMDD symptoms. Patients can take selective serotonin reuptake inhibitors (SSRIs) specifically for only a few days, timed to their menstrual cycles. Typical recommendations for the intake of antidepressants assume a longer period of medication.
In principle, serotonin levels can also be influenced by eating habits, says Julia Sacher. “Precursor substances of serotonin, such as tryptophan, can be found for example in cheese, poultry, soy beans, tofu, nuts and dark chocolate. Especially in winter, when reduced hours of sunlight and gloomy weather can contribute to a worsening of mood, it makes sense to pay some attention to what you eat. A daylight lamp can also positively affect the serotonin balance.
“However, these measures do not reach the concentrations that can, and sometimes need to be achieved through medication. Future studies need to investigate PMDD symptoms can specifically be influenced through diet and light therapy.”
The study is published in Biological Psychiatry.
More information:
Julia Sacher et al, Increase in serotonin transporter binding in patients with premenstrual dysphoric disorder across the menstrual cycle: a case-control longitudinal neuroreceptor ligand PET imaging study, Biological Psychiatry (2023). DOI: 10.1016/j.biopsych.2022.12.023
Journal information:
Biological Psychiatry
Source: Read Full Article