Pregnancy is recognized to be a high-risk condition for complications associated with infection by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). As a result, many healthcare providers have turned to monoclonal antibodies (mAbs) to mitigate the severity of the coronavirus disease 2019 (COVID-19) in this population, as in others.
In a recent Infection study, researchers examine the safety and efficacy of mAbs in pregnant and postpartum women.

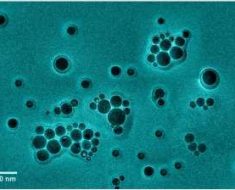
Study: Treatment with Anti-SARS-Cov-2 Monoclonal Antibodies in Pregnant and Postpartum Women: First Experiences in Florence, Italy. Image Credit: Evgeniy pavlovski / Shutterstock.com
Introduction
Pregnant women diagnosed with COVID-19 are at more than twice the risk of death, and almost 20 times the risk of intensive care unit (ICU) admission as compared to non-pregnant women with COVID-19. Furthermore, newborns born to SARS-CoV-2-infected mothers have five times higher odds of requiring neonatal intensive care unit (NICU) care after birth.
The use of mAbs to treat COVID-19 has gradually increased since their approval. Early recommendations were to prevent disease progression, which reserved mAbs to primarily be used to treat high-risk patients with mild to moderate COVID-19 within ten days of symptom onset. At present, mAbs are being extended to patients hospitalized with COVID-19.
The National Health Institute (NIH) of Italy has recommended that pregnant women receive mAbs for the same indications as non-pregnant women, particularly in the presence of high-risk factors. It should be noted that pregnancy is associated with altered immune function.
Considering the poorer outcomes associated with COVID-19 in pregnancy and current recommendations, physicians at the Careggi University Hospital in Florence, Italy have offered mAbs to all pregnant COVID-19 outpatients with mild to moderate disease.
The current study presents early results with this practice, in light of scarce data about mAb use during pregnancy.
Study findings
During the study period, from March 1, 2020, to September 30, 2020, ten pregnant patients were treated for COVID-19. Two did not require hospitalization, and three who were hospitalized were incidentally found to have COVID-19. These five patients were given 2.4 g casirivimab/imdevimab.
Conversely, five pregnant women who were hospitalized for COVID-19 but seronegative at admission were also given 8 g of casirivimab/imdevimab.
Four patients had a body mass index (BMI) over 25. All patients had one or more symptoms of COVID-19 at the time of presentation, and genomic sequencing data showed that all were infected with the SARS-CoV-2 Delta variant. Six patients had moderate symptoms, whereas four were reported to have severe COVID-19 at the time of mAb administration.
Taken together, mAbs were well tolerated. All outpatients recovered rapidly, being treated only with ibuprofen on a symptomatic basis.
Inpatients were put on the anticoagulant enoxaparin until discharge. Four required low-flow oxygen, whereas three patients also received steroids.
One of the three inpatients with an incidental diagnosis of COVID-19 developed severe respiratory failure; however, this patient ultimately recovered and was discharged without the need for additional oxygen supplementation. One patient had myocarditis during admission that was attributed to the infection.
No mortalities and no intensive care unit admissions were reported. All eight hospitalized patients did not require oxygen supplementation at discharge, which occurred at a median of seven days.
At 28 days, clinical recovery was universal. Delivery was uncomplicated in five patients, two had preterm births, one due to pre-eclampsia at 36 weeks, and one due to premature rupture of membranes at 34 weeks gestation.
Two Cesarean sections were performed, one in the aforementioned pre-eclamptic patient and one due to a high-risk cardiotocography test. In the latter case, the baby appeared healthy at birth.
None of the babies born to treated mothers had significant events attributable to the mAbs or maternal COVID-19. All newborns were permitted to breastfeed.
Implications
The results of this small study corroborate earlier reports that confirm mAbs to be safe and effective in treating pregnant COVID-19 patients. Immunoglobulin use in pregnancy is not new, as it has been used to prevent hemolytic disease of the newborn due to maternal/fetal Rh incompatibility.
Both patients in pregnancy and those in the immediate post-partum period were included in this study, as both were considered to be experiencing the same effects induced by the pregnant state. In fact, the patient who developed the most severe symptoms was in the immediate postpartum.
Pregnant patients with COVID-19 are typically healthy, thereby indicating that pregnancy may predispose these patients to SARS-CoV-2 infection and more severe disease. This could be due to the immunomodulation that occurs during pregnancy, which can lead to an enhanced inflammatory response to the infection.
The findings of the current study indicate that SARS-CoV-2 mAbs can be safely used in pregnant COVID-19 outpatients. However, the recent rise of the Omicron variant has made this particular combination of mAbs obsolete, due to the presence of numerous escape mutations. Therefore, when Omicron accounts for over 80% of cases, casirivimab/imdevimab administration is contraindicated.
Sotrovimab is another mAb that has shown in vitro efficacy against Omicron and may prove useful if these results are validated clinically.
In conclusion, our experience suggests that mAbs against SARS-CoV-2 can be a safe tool to treat pregnant and postpartum patients in the first phases of the disease, or seronegative patients hospitalized for COVID-19.”
- Manciulli, T., Modi, G., Campolmi, I., et al. (2022). Treatment with Anti-SARS-Cov-2 Monoclonal Antibodies in Pregnant and Postpartum Women: First Experiences in Florence, Italy. Infection. doi:10.1007/s15010-022-01777-z.
Posted in: Medical Research News | Medical Condition News | Women's Health News | Disease/Infection News
Tags: Antibodies, Anticoagulant, Baby, Body Mass Index, Coronavirus, Coronavirus Disease COVID-19, Eclampsia, Efficacy, Genomic, Genomic Sequencing, Healthcare, Hospital, Ibuprofen, Immunoglobulin, in vitro, Intensive Care, Myocarditis, Neonatal Intensive Care, Newborn, Omicron, Oxygen, Pre-eclampsia, Pregnancy, Respiratory, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Sotrovimab, Syndrome

Written by
Dr. Liji Thomas
Dr. Liji Thomas is an OB-GYN, who graduated from the Government Medical College, University of Calicut, Kerala, in 2001. Liji practiced as a full-time consultant in obstetrics/gynecology in a private hospital for a few years following her graduation. She has counseled hundreds of patients facing issues from pregnancy-related problems and infertility, and has been in charge of over 2,000 deliveries, striving always to achieve a normal delivery rather than operative.
Source: Read Full Article