Save articles for later
Add articles to your saved list and come back to them any time.
Tucked away in the corner of a third floor in the Mercy Hospital for Women is a clinic few people know about. Every patient here has suffered the heartbreak of miscarriage and stillbirth.
The waiting room of the STAR (Stillbirth and Reproductive Loss) Clinic in Heidelberg in Melbourne’s northeast is filled with women hoping for news of an imminent pregnancy or a pregnancy that’s still healthy.
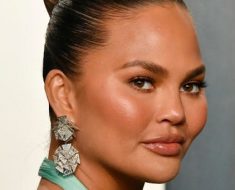
Dr. Liz McCarthy from the STAR Clinic.Credit: Simon Schluter
For nine anxiety-ridden months I was a STAR patient, having lost two previous pregnancies – a miscarriage at nine weeks and a stillbirth, Evie Michelle, at 20 weeks.
Surviving subsequent pregnancy after loss is like running a marathon with your eyes glued to the ground. One foot falling after another, never daring to take a look at the finish line for fear of more shock and heartbreak.
For my family, Evie’s death in October 2020 wasn’t just the loss of a human who never was. She already had a seat at our table, a childhood, a career, a place in our hearts.
There are many delicacies that surround women and their partners after miscarriage, stillbirth and terminations for medical reasons (TFMR). The question of whether to try again is often mired in fear.
As my husband put it at the time, getting pregnant again was ‘the last roll of the dice’. Fortunately for us it resulted in the healthy birth of Evelyn, named in honour of her older sister, in August last year.
An estimated 86 per cent of women become pregnant again within 18 months following perinatal loss, according to a 2017 study published in the Journal of Psychosomatic Obstetrics and Gynaecology.
However, their grief makes the experience of pregnancy more daunting and mentally taxing, which is why Dr Elizabeth McCarthy set up the STAR clinic in 2009.
Unlike clinics in other hospitals that offer high-risk counselling or debrief sessions after loss, STAR is the only clinic in Melbourne to care for women in what Dr McCarthy calls ‘a one-stop shop’.
Dr Liz McCarthy from the Mercy Hospital for Women, with author Kate Jones and her daughter Evelyn Hague.Credit: Simon Schluter
With a team of obstetricians, midwives and psychologists, it offers specialist pre-pregnancy advice, investigation and extra support during the woman’s next pregnancy.
“It was primarily just me, once a week with an ultrasound, and I would see women who’d had three or more early miscarriages or a mid-trimester or later pregnancy loss,” McCarthy explained.
“Then it became more multidisciplinary and we integrated what’s called liaison psychiatry. We think, but it’s hard to prove, that it probably reduces the stigma of having mental health involvement and also helps with that feeling that people tell me they’re worried they’re going mad because they feel so sad.”
McCarthy says she sees more of the happier stories, but the women who come through her clinic carry the loss of babies they never got to hold.
“I can remember individuals that stopped trying to have a baby after a few cases. I think one was 14 [pregnancies], one [had] seven, one nine, that I know for definite just couldn’t go on, and nature didn’t give them the baby they were hoping for,” she says.
“Because I’ve been in this for the long game, I’ve certainly met women who’ve had up to 21 pregnancies… that particular woman is now expecting her fourth baby and I think that’s going to be positive. [But] it’s a burden that she still carries with her, all of those losses.”
Kellie Hermann first came to the STAR Clinic during her fifth pregnancy, having had four miscarriages before eight weeks. She experienced four more miscarriages before having Mia in 2019 and she is now expecting a baby boy in early July.
“The reason I fell into STAR is someone recommended I go to the Mercy for the management of a loss and that’s when I started to have the investigation work done there and I felt really supported every time I went,” she says.
“If anyone is ever going to tell me that my baby doesn’t have a heartbeat, I want it to be Liz or one of her team because they are so caring and they have so much experience.”
The reasons behind pregnancy loss are varied and complex, ranging from polycystic ovary syndrome to infection. In addition to researching these reasons, more experts are turning their attention to helping women become pregnant afterwards.
Dr Alex Heazell, a professor of obstetrics at the University of Manchester, founded the first Rainbow Clinic in the UK to help care and support for parents who have suffered a stillbirth or neonatal death. There are now 27 Rainbow Clinics across the UK and three in the US.
“STAR clinic has been doing some pioneering work in Australia in the same way our Rainbow Clinic has in Manchester,” he says.
“I think the really nice thing is the wider maternity community are now realising that and there’s quite a lot of interest in pregnancy-after-loss clinics and how they might improve women’s
experiences of care.”
McCarthy says the hope of a “rainbow child” keeps many women going.
“I think hope is such a strong thing for women. Even a lot of them, even when they are grieving the child they’ve lost, they also are aware of themselves as a potential life giver.”
Make the most of your health, relationships, fitness and nutrition with our Live Well newsletter. Get it in your inbox every Monday.
Most Viewed in Lifestyle
From our partners
Source: Read Full Article