Billions of microorganisms, including bacteria, fungi, and archaea, are present in the human nose, which collectively form the nasal microbiome.
Several studies have indicated that the nasal microbiome is an important factor for personal and global health. In fact, considerable evidence has been reported regarding the links between the gut microbiome and Parkinson’s disease (PD). Some studies have also indicated that signals from nasal microbiota reach the brain through the olfactory system and affect the nervous system function.

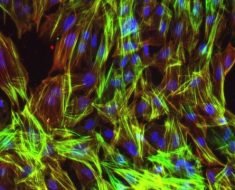
Study: The microbiome–nose–brain axis in health and disease. Image Credit: goa novi / Shutterstock.com
A recent Trends in Neurosciences study provides an overview of how the nasal bacterial population influences olfactory processing and neurodegeneration, particularly in Parkinson’s disease (PD).
Composition of the nasal microbiome
Among the different microorganisms that are present in the nose, bacteria are considered the main component. Although 104 different strains of bacteria are present in the nose, only two to ten species make up 90% of an individual’s nasal microbiome. Most of the bacterial strains are symbiotic; however, some opportunistic pathobionts are also present that may cause various illnesses.
Colonization of symbiotic microbes has been detected since birth that continues to develop during the first year of life. Firmicutes and Proteobacteria are abundantly present in children, whereas Actinobacteria are over-represented in adults.
Bacterial pathogens, such as Haemophilus influenzae, Moraxella catarrhalis, and Streptococcus pneumoniae, are also occasionally detected in nasal microbiota. These bacteria have the potential to cause upper respiratory tract infections.
The bacterial composition associated with the nasal microbiome of an individual is influenced by geographical factors, proximity to animals, climate, drinking water composition, air quality, diet, and prevalence of infectious diseases. Additionally, the age and immunity of the host are also major determining factors that influence nasal microbiota composition.
The role of the nasal microbiome in olfaction
Several studies have indicated that the nasal microbiota limits pathogenic colonization and modulates host-immune responses associated with respiratory tract infections and disease severity. However, a limited number of studies related to the role of the nasal microbiome in olfactory performance have been conducted.
In vivo experiments using a mouse model revealed that the nasal microbiome has a vital role in the nasal epithelium function as odorant responses. A stronger and more rapid odorant response was recorded through electroolfactogram in germ-free mice.
The amplitude and speed of odorant-evoked responses were different based on odorant nature in nasal microbiota-free mice. Therefore, alterations in the nasal microbiome could significantly affect the health of an individual due to the influence of olfaction on both nutrition and general health.
Odorants are sensed by olfactory sensory neurons (OSNs) in mammals. OSNs are present in the olfactory epithelium of the posterior nasal cavity.
To determine whether nasal microbiota impacts human olfaction, 18 to 46-year-old individuals in a previous study were classified into three groups: good, normal, and poor sense of smell. This study revealed that although a similar nasal microbial population was present in all groups, the presence of butyric-acid-producing bacteria in the nasal microbiome caused alterations in the olfactory functions.
Nasal microbiota and neurodegenerative diseases
OSNs are extremely vulnerable to external factors, including toxins like herbicides and pesticides, as well as other microorganisms like coronaviruses and Staphylococcus. These factors can lead to mitochondrial damage, inflammation-induced axon damage, and oxidative stress. These changes can modify OSNs and, as a result, cause dysfunction of the olfactory bulb.
Olfactory deficits can occur due to differential nasal bacterial colonization. Olfactory deficits are closely associated with neuroinflammation, inflammation, and neurodegenerative diseases such as Zika, coronavirus disease 2019 (COVID-19), PD, and Alzheimer’s disease.
PD is a neurodegenerative disease that is characterized by the loss of dopaminergic neurons in the substantia nigra.
The current study discusses how the nasal microbiome impacts the incidence and prognosis of PD. Olfactory dysfunction has been observed in the early phase of PG progression. Thus, it has been assumed that the nasal microbiome may influence the neuronal accumulation of misfolded OSNs.
In most PD patients, misfolded alpha-synuclein (aSyn) is a vital component of Lewy bodies that is considered to be a marker of PD. Chronic nasal dysbiosis induced by local inflammation can significantly enhance neurodegenerative damage of OSNs, which leads to an accumulation of misfolded aSyn.
This pathological condition might progress to the olfactory bulb and significantly impact cognitive, motor, and psychiatric expressions in PD patients. Misfolded aSyn commonly appears in the olfactory bulb tissue and neuroepithelium samples of PD patients.
In a recent U.S.-based study, nostril swabs collected from endoscopies showed that nasal dysbiosis is strongly associated with PD. Herein, a distinct nasal microbiome was found in PD patients as compared to healthy individuals.
The nasal microbiome of PD patients is characterized by an increased concentration of bacteria belonging to the phylum Proteobacteria. Nevertheless, many studies contradict the finding of this study and report that no significant difference in the nasal microbiome was observed between PD patients and controls.
Conclusions
Nasal dysbiosis leads to aSyn aggregation, which has been associated with neurodegenerative processes. In the future, more research is needed to better elucidate the role of the microbiome-nose-brain axis in the development and progression of PD.
- Lazarini, F., Roze, E., Lannuzel, A., & Lledo, P. (2022) The microbiome–nose–brain axis in health and disease. Trends in Neurosciences. doi:10.1016/j.tins.2022.08.003
Posted in: Medical Science News | Medical Research News | Medical Condition News | Disease/Infection News
Tags: Archaea, Bacteria, Brain, Cell, Children, Chronic, Coronavirus, covid-19, Diet, Dopaminergic, Dysbiosis, fungi, Global Health, Herbicides, immunity, in vivo, Infectious Diseases, Inflammation, Lewy Bodies, Microbiome, Mouse Model, Nervous System, Neurodegeneration, Neurodegenerative Disease, Neurodegenerative Diseases, Neurons, Nutrition, Olfaction, Oxidative Stress, Parkinson's Disease, Pesticides, Research, Respiratory, Respiratory Tract Infections, Streptococcus pneumoniae, Stress, Toxins

Written by
Dr. Priyom Bose
Priyom holds a Ph.D. in Plant Biology and Biotechnology from the University of Madras, India. She is an active researcher and an experienced science writer. Priyom has also co-authored several original research articles that have been published in reputed peer-reviewed journals. She is also an avid reader and an amateur photographer.
Source: Read Full Article