TOPLINE:
The pancreatic effects of the “twincretin” tirzepatide (Mounjaro) appear to depend at least as much on the drug’s agonist activity on the glucose-dependent insulinotropic polypeptide (GIP) receptor as on its glucagon-like peptide-1 (GLP-1) receptor activity.
METHODOLOGY:
-
The researchers determined which incretin receptor (GLP-1 or GIP) tirzepatide uses to stimulate insulin secretion in isolated human pancreatic islet cells from donors. Donors could be of either sex, and body mass index, age, and A1c levels varied.
-
Study protocols ran in vitro on such cells from human donors who did not have diabetes and who had a broad range of metabolic characteristics.
-
The investigators also determined which incretin receptor plays the major role in stimulating glucagon secretion from isolated human pancreatic islet cells.
TAKEAWAY:
-
The data show that tirzepatide stimulates islet hormone secretion from human islets through agonist effects at both incretin receptors (GIP and GLP-1).
-
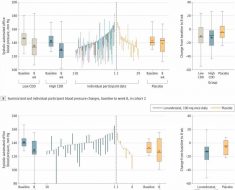
Antagonizing the GLP-1 receptor failed to reduce tirzepatide-stimulated insulin secretion, but antagonizing the GIP receptor reduced insulin secretion by about 55%.
-
Antagonism of the GIP receptor consistently decreased tirzepatide-stimulated insulin secretion across all donor islet cell samples, while the impact of GLP-1 receptor antagonism varied among islet preparations.
-
In isolated human islets, the researchers confirmed that human GIP stimulated glucagon secretion, human GLP-1 decreased glucagon secretion, and the combination of the two was offsetting to produce a rate of glucagon secretion that matched unstimulated levels.
-
GIP receptor agonism appears important for inducing both insulin and glucagon secretion from isolated human pancreatic islet cells.
IN PRACTICE:
“The data clearly demonstrate that in isolated human islets, tirzepatide requires the GIP receptor to stimulate both insulin and glucagon secretion,” the authors conclude. However, they add: “It is important to note that although the human islets we utilized came from donors with a broad range of metabolic characteristics, we did not have the opportunity to include islets from donors with type 2 diabetes.”
STUDY DETAILS:
The study’s lead researchers were based at Duke University in Durham, North Carolina, the German Center for Diabetes Research in Neuherberg, Germany, and at Eli Lilly, the company that markets tirzepatide (Mounjaro). The study appears in Nature Metabolism.
LIMITATIONS:
Similar in vivo studies involving people with and those without diabetes are needed.
DISCLOSURES:
Several researchers receive funding from Novo Nordisk and Eli Lilly. Several co-authors are employees of either Eli Lilly or Novo Nordisk. One co-author served as a consultant or speaker for Eli Lilly and Structure Therapeutics; a second author served as a consultant or speaker for Structure Therapeutics. The remaining authors have disclosed no relevant financial relationships.
Mitchel L. Zoler is a reporter with Medscape and MDedge based in the Philadelphia region. @mitchelzoler
For more diabetes and endocrinology news, follow us on Twitter and on Facebook.
Source: Read Full Article