In a recent study published in PLOS, researchers determined whether the incidence of new diabetes mellitus (DM) and cardiovascular diseases (CVDs) increases in a year among those recovering from coronavirus disease 2019 (COVID-19).

Background
Some early COVID-19-induced cardiac manifestations detected in the first four weeks of infection include heart failure, acute myocardial infarction, and ischemic stroke. Additionally, COVID-19 patients have reported new-onset hyperglycemia and DM cases, with diabetic ketoacidosis and hyperosmolarity.
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) likely causes direct pancreatic damage. Additionally, it triggers a proinflammatory 'cytokine storm' in severely-ill patients characterized by increased interleukin-6 (IL-6) and tumor necrosis factor-alpha (TNFα) levels that impairs insulin secretion and resistance. In a nutshell, COVID-19 heightens the risk of blood glucose disorders and cardiovascular complications. However, studies have barely investigated and characterized new diagnoses of DM and CVDs over 12 months after COVID-19.
Social restrictions during the pandemic made profound changes in people's dietary and exercise routines that might have caused CVD and DM in the general population without COVID-19. Therefore, there is a need for controlled studies that carefully evaluate the long-term impacts of SARS-CoV-2 infection and its cardiometabolic outcomes accounting for pre-existing health conditions in cases and controls and its variations over time in the control cohort.
Also, cohort studies should clarify the distinction between adverse cardiometabolic outcomes that occur during acute (first four weeks of infection), post-acute (five to 12 weeks after the first infection), or long-COVID with symptoms persisting for more than 12 weeks after infection.
About the study
In the present study, researchers analyzed electronic health records (EHRs) of 428,650 COVID-19 patients without CVD or DM between 2020 and 2021 in the United Kingdom (UK). The index date was the date of the first code for COVID-19 in the February 2021 release of Clinical Practice Research Datalink (CPRD) Aurum. The database includes EHRs of 1,356 family practices in the UK with around 13.4 million registered patients, per their March 2022 release.
The study population comprised an equal number of test and control patients matched 1:1 based on age, gender, and family practice. Other study co-variates included body mass index (BMI), Charlson score, systolic blood pressure, and index month. The team followed up with the study population up to January 2022; they divided the yearlong study into three-time frames from the index date, as follows: i) first four weeks, ii) five to 12 weeks, iii) 13 to 52 weeks.
The primary study outcomes were the first record of CVD and DM diagnoses. The researchers categorized CVD diagnoses into multiple categories, as follows: i) atrial arrhythmias, including atrial fibrillation and supraventricular tachycardia, ii) heart attack, iii) myocardial infarction and ischaemic heart disease, iv) pulmonary embolism, v) venous thrombosis, vi) cardiomyopathy and myocarditis, and vii) stroke.
Likewise, DM diagnoses had two broad categories – individuals with type 1 and 2 DM and those receiving hypoglycemic drugs orally and insulin. The team considered the second record of hemoglobin A1c (HbA1c) greater than equal to 48 mmol/mol diagnostic of diabetes. They evaluated mortality from the CPRD date of death.
Study findings
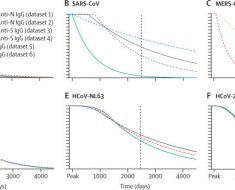
The net DM diagnoses increased in the first four weeks after COVID-19 by 81%, with an adjusted rate ratio (RR) of 1.81, and remained elevated between five to 12 weeks (RR=1.27). However, the overall increase in DM diagnoses could not sustain between 13 to 52 weeks (R=1.07). Further, the authors observed a six-fold rise in CVD diagnoses with acute COVID-19 (RR=5.82). Additionally, they observed an 11-fold increase in pulmonary embolism, a six-fold increase in atrial arrhythmias, and a five-fold increase in venous thromboses, with RRs of 11.51, 6.44, and 5.43, respectively. Notably, the CVD incidence decreased between five to 12 weeks of initial SARS-CoV-2 infection (RR=1.49) and attained baseline levels or below between 12 weeks and 12 months, with RR=0.80.
Conclusions
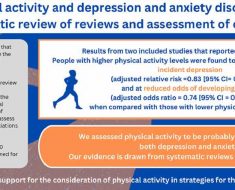
The current study findings showed that while CVD increased early after COVID-19, DM diagnoses remained elevated for a minimum of 12 weeks following COVID-19 before decreasing again. The authors observed that the initial surge in CVD diagnoses was mainly due to pulmonary embolism, atrial arrhythmias, and venous thromboses. Individuals without pre-existing CVD or DM who contracted COVID-19 showed no increased susceptibility towards the incidence of both these conditions. The authors stressed a healthy diet and exercise for individuals recovering from COVID-19.
- Emma Rezel-Potts, Abdel Douiri, Xiaohui Sun, Phillip J. Chowienczyk, Ajay M. Shah, Martin C. Gulliford. (2022). Cardiometabolic outcomes up to 12 months after COVID-19 infection. A matched cohort study in the UK. PLOS. doi: https://doi.org/10.1371/journal.pmed.1004052 https://journals.plos.org/plosmedicine/article?id=10.1371/journal.pmed.1004052
Posted in: Medical Science News | Medical Research News | Disease/Infection News
Tags: Atrial Fibrillation, Blood, Blood Pressure, Body Mass Index, Cardiometabolic, Cardiomyopathy, Coronavirus, Coronavirus Disease COVID-19, covid-19, Cytokine, Diabetes, Diabetes Mellitus, Diabetic Ketoacidosis, Diagnostic, Diet, Drugs, Embolism, Exercise, Glucose, HbA1c, Heart, Heart Attack, Heart Disease, Heart Failure, Hemoglobin, Hyperglycemia, Insulin, Interleukin, Interleukin-6, Ischaemic Stroke, Mortality, Myocardial Infarction, Myocarditis, Necrosis, Pandemic, Pulmonary Embolism, Research, Respiratory, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Stroke, Syndrome, Thrombosis, TNFα, Tumor, Tumor Necrosis Factor

Written by
Neha Mathur
Neha is a digital marketing professional based in Gurugram, India. She has a Master’s degree from the University of Rajasthan with a specialization in Biotechnology in 2008. She has experience in pre-clinical research as part of her research project in The Department of Toxicology at the prestigious Central Drug Research Institute (CDRI), Lucknow, India. She also holds a certification in C++ programming.
Source: Read Full Article