While older adults, defined as those 65 and older, make up the largest percentage of cancer patients and survivors, this group is not adequately represented in clinical trials, research at the University of Cincinnati has shown.
This low representation is further complicated by the underreporting of the treatment efficacy and adverse effects specific to older adults, according to research led by Karlynn BrintzenhofeSzoc of the UC College of Allied Health Sciences. The study concludes that conscious efforts are needed to address these deficiencies which could lead to improved treatment decisions and outcomes for older adults with cancer.
“In 2015, an article in the Journal of Clinical Oncology found that evidence-based treatment protocols for treating older adults with cancer is totally lacking,” says BrintzenhofeSzoc. “The Food and Drug Administration (FDA), the National Clinical Cancer Institute and other research groups are pushing to get older adults into clinical trials. As a result, they’re starting to be seen and treated in clinical trials, but not reported on.”
BrintzenhofeSzoc got involved in this research after being asked to join the Cancer and Aging Research Group, an international grassroots organization whose mission is to join geriatric oncology researchers across the nation in a collaborative effort of designing and implementing clinical trials to improve the care of older adults with cancer.
BrintzenhofeSzoc and the other researchers set out to examine the current state of the art in phase III chemotherapeutic clinical cancer trials in reporting about older adults. They studied one year’s worth of literature, from July 1, 2016, to June 30, 2017. The first pass at that resulted in a match of 929 articles; however, more than 600 of those didn’t meet the study group’s inclusion criteria, while another 116 were duplicates.
At the completion of the elimination process, the group was left with 159 articles to review. BrintzenhofeSzoc says she read every single title and abstract of all 929 articles, making a decision on whether it met the criteria and then shared it with the nine other reviewers in the group, made up of people with a wide range of experience and expertise. It included social workers like BrintzenhofeSzoc as well as oncologists, gerontologists, medical and doctoral students, health scientists and a librarian.
“When we finally finished analyzing all of the articles, we found the evidence on how you treat older adults with cancer is terrible,” says BrintzenhofeSzoc. “There’s no evidence-based guidelines, which goes against the current focus on precision and evidence-based medicine to help treat older adults with cancer.”
BrintzenhofeSzoc says the group aims to get researchers to separate out different aged groups of people in trials and examine how they are different in efficacy and in side effects or adverse events. That would allow the medical community to implement treatment protocols that take into account evidence-based research results in patients with different types of cancer and of younger and older patients.
She says one of the major debates in science currently is defining exactly the age of an older adult.
“The American Cancer Society and the FDA have been using the cutoff of an older adult being equal to or greater than 65 years old,” she says. “There’s a lot of discussion of moving it to 70 or higher. There needs to be some consistency. It’s not about a chronological age, it is about what your body looks like, what you’ve done, how you’ve developed. This goes to social determinants of health and behavioral lifestyles.”
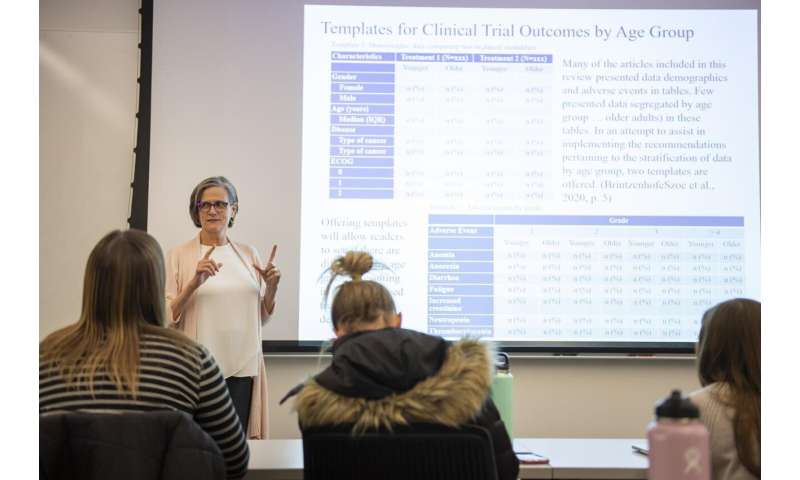
The paper reporting the research was published in the Journal of Geriatric Oncology in January 2020 and includes two templates designed by the research team. One focuses on demographic data comparing two treatment methods, while the other examines adverse events by grade, with a grade of one being the least severe and four the most severe. The adverse events include anemia, anorexia, diarrhea and fatigue. The templates were developed after examining all 159 papers that met the criteria and finding some disturbing similarities.
“What we found was that it’s like someone wrote the first clinical trial article decades ago and everyone has followed that format exactly,” she says. “You know exactly where to find what. The tables are almost exactly alike across every article.”
BrintzenhofeSzoc hopes the templates are widely put into practice, but she estimates it is going to take three to five years to know how impactful they are.
Source: Read Full Article





