Cardiovascular health (CVH) scores that include sleep predicted CV disease risk among older US adults, supporting the American Heart Association (AHA)’s recent inclusion of sleep in its own checklist.
Sleep duration is now considered “an essential component for ideal heart and brain health,” according to the AHA’s updated checklist, now called Life’s Essential 8.
“Our study is the first to show that sleep metrics add independent predictive value for CVD events over and above the original seven cardiovascular health metrics, providing support for updating the guidelines from Life’s Simple 7 (LS7) to Life’s Essential 8,” lead author Nour Makarem, PhD, of the Mailman School of Public Health at Columbia University Irving Medical Center in New York City, told theheart.org | Medscape Cardiology.
For the study, her team compared four versions of LS7 checklists that included sleep in relation to cardiovascular disease (CVD) risk.
“CVH scores that included sleep duration alone as a measure of overall sleep health, as well as scores that included multiple dimensions of sleep health (i.e., sleep duration, efficiency, and regularity, daytime sleepiness, and sleep disorders), were both predictive of future CVD,” she said.
Study participants scoring in the highest tertile of the CVH checklists that included sleep had up to a 47% lower CVD risk.
Sleeping 7 hours or more but less than 9 hours nightly was considered “ideal,” according to the study, which was published online October 19 in the Journal of the American Heart Association.
Lower the Odds
Makarem and colleagues analyzed data from participants in the Multi-Ethnic Study of Atherosclerosis (MESA) sleep study using overnight polysomnography, 7-day wrist actigraphy, validated questionnaires, and outcomes. They used the data to evaluate the four iterations of an expanded LS7 score:
-
Score 1 included sleep duration;
-
Score 2 included sleep characteristics linked to CVD in the literature (sleep duration, insomnia, daytime sleepiness, and obstructive sleep apnea [OSA]);
-
Score 3 included sleep characteristics associated with CVD in MESA (sleep duration and efficiency, daytime sleepiness, and OSA); and
-
Score 4, also based on CVD in MESA, included sleep regularity.
Among 1920 participants (mean age 69 years; 54% women; 40%, White individuals), the mean LS7 score was 7.3, and the means of the alternate CVH scores that included sleep ranged from 7.4 to 7.8 (scores range from 0 to 14, with higher scores indicating better CVH).
On actigraphy, 63% of participants slept less than 7 hours; 30% slept less than 6 hours; 39% had high night-to-night variability in sleep duration; and 25% had high variability in sleep onset timing.
Overall, 10% had sleep efficiency less than 85%; 14% had excessive daytime sleepiness; 36% had high insomnia symptoms; and 47% had moderate to severe OSA. Short-duration sleepers also had a higher prevalence of overweight/obesity, diabetes, and hypertension and had lower mean LS7 scores.
During a mean follow-up of 4.4 years, 95 prevalent CVD events and 93 incident cases occurred.
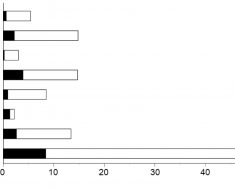
Higher scores on all four expanded versions were related to lower odds of having CVD. Participants in the highest vs the lowest tertile of the LS7 score had 75% lower CVD odds (odds ratio [OR], 0.25). Similarly, those in the highest vs the lowest tertile of CVH scores 1 and 2 had 71% and 80% lower odds of prevalent CVD (OR, 0.29 and OR, 0.20), respectively.
Overall, participants in the highest vs lowest tertile of the LS7 score and all CVH scores had up to 80% lower odds of prevalent CVD; those in the highest vs lowest tertile of CVH score 1, which included sleep duration, and CVH score 4, which included multidimensional sleep health, had 43% and 47% lower incident CVD risk (hazard ratios [HRs] 0.57 and 0.53), respectively.
The LS7 score alone was not significantly associated with CVD incidence (HR, 0.62).
“Clinicians should ask patients about their sleep health and emphasize the importance of prioritizing sleep for heart disease prevention,” Makarem said.
Sleep ‘Devalued’
“The sleep field has been fighting to get more sleep education into medical education for decades,” AHA volunteer expert Michael A. Grandner, PhD, Director of the Sleep & Health Research Program and of the Behavioral Sleep Medicine Clinic at the University of Arizona College of Medicine in Tucson, told theheart.org | Medscape Cardiology.
“To my knowledge, there still is not a lot of attention given to it, partly because the culture in medical school and among residents is one of not sleeping,” said Grandner, who was not involved in the study. “The culture among physicians is ‘Who needs sleep? I function fine without it.'”
“Sleep made it to the checklist because it is a biological requirement for human life,” he noted. “We sleep for the same reason we breathe and drink. It’s an imperative. Yet we live in a society that devalues sleep.”
It’s “extremely unusual” for a doctor to ask a patient how they’re sleeping, he said. “It’s also pretty unusual to have sleep-related conversations between doctors and patients, especially in the context of health, not just, ‘Hey, doc, I can’t sleep, throw me a pill.'”
Clinicians should be asking every patient about how they’re sleeping at every visit, Grandner said. “It’s now part of the official definition of heart health. Just like you would be remiss if you didn’t ask about smoking or test blood pressure, you’d be missing something important by not asking about sleep — something that has similar billing to diet, exercise, blood pressure, and all the other ‘essentials.'”
No commercial funding or conflicts of interest were declared.
J Am Heart Assoc. Published online October 19, 2022. Full text
Follow Marilynn Larkin on Twitter: @MarilynnL.
For more from theheart.org | Medscape Cardiology , follow us on Twitter and Facebook
Follow Medscape on Facebook, Twitter, Instagram, and YouTube
Source: Read Full Article