Why isn’t the NHS using private hospitals to clear the surgery backlog? The move could mean 30,000 extra ops a month and wouldn’t cost more money
For two years, Joseph Togher had been unable to walk for more than a few minutes without searing pain in his legs — ‘like electricity running down them’ — which left the 72-year-old from Blackpool virtually housebound.
After an MRI scan last March, it was clear he needed surgery to free a pinched nerve in his spine.
This was when the NHS was in the midst of dealing with the Covid pandemic and millions of patients were facing long delays for treatment.
But Joseph was told that rather than the year-long wait he faced in an NHS hospital, he could have the operation within weeks — thanks to an arrangement with a local private hospital.
Just ten weeks after seeing an NHS consultant in July 2021, he had the two-hour procedure which was not only a success but was carried out in ‘five-star’ surroundings, says Joseph, a retired acupuncturist and ice cream van owner.

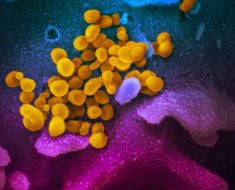
Joseph was told that rather than the year-long wait he faced in an NHS hospital, he could have the operation within weeks — thanks to an arrangement with a local private hospital. A file photo is used above
‘I was so lucky to have the opportunity to go to the private hospital — I can’t praise them enough.’
More than six million people — the equivalent of 10 per cent of the population of England — are currently awaiting NHS treatment, thanks to the knock-on effects of the pandemic.
Many thousands have endured a two-year delay in operations for hip or knee replacements, or cataract surgery. Yet there seems to be a simple solution.
Good Health has been told that private hospitals in the UK have the capacity to do ‘at least 30 per cent more than they did pre-pandemic’ — equivalent to about 30,000 more procedures a month, giving tens of thousands of patients the treatment they need.
The 30,000 figure is based on an analysis of NHS performance by the Independent Healthcare Providers Network (IHPN), which represents private hospitals and clinics in the UK. One network of private cancer clinics even says that it could almost triple the number of NHS cancer treatments it provides ‘overnight’, if given the go-ahead.
‘The NHS currently uses about 30 per cent of our capability, but we could boost the number of treatment sessions for NHS patients to above 80 per cent, offering many thousands of treatments for NHS patients,’ says Sean Sullivan, CEO of Rutherford Health, which has five private cancer centres across the UK.

Latest figures show that more than 99,000 treatments were carried out on NHS patients in private hospitals in February 2022 — still below pre-pandemic levels of roughly 105,000 procedures every month. A file photo is used above
Crucially, the cost would be no greater than treating the patients on the NHS. NHS pricing rules state that independent providers are paid the NHS price for NHS work, which is invariably lower than private clinics would normally charge. These private sector offers seem like a no-brainer.
They also mirror the NHS ambition, set out in the Delivery Plan for Tackling the Covid-19 Backlog of Elective Care, published in February, to be delivering about 30 per cent more routine procedures by 2024/25. According to private hospitals, there is plenty of spare capacity for the NHS to use.
Latest figures show that more than 99,000 treatments were carried out on NHS patients in private hospitals in February 2022 — still below pre-pandemic levels of roughly 105,000 procedures every month. Increasing this pre-pandemic level by 30 per cent would mean an extra 30,000 could be done a month.
David Hare, chief executive of the IHPN, says: ‘Given the scale of the backlog, it’s vital an “all shoulders to the wheel” approach is taken to tackle NHS waiting lists.
‘The independent health sector is a vital tool in the NHS’ armoury to bring down waiting times.’
Last December, Rutherford Health offered NHS England a ‘three-year not-for-profit deal’ to use more than 80 per cent of its capacity to help tackle the NHS cancer backlog. Currently, the NHS uses about 30 per cent.
As it explained in a letter seen by Good Health, the increase to 80 per cent would amount to 13,500 chemotherapy sessions, 18,072 radiotherapy sessions, more than 6,000 proton beam sessions (a new more precise type of radiotherapy), 20,000 MRI, 18,000 CT and 24,000 ultrasound scans a year.
‘We have fully staffed new units which could take patients from the NHS waiting list straight away,’ says Sean Sullivan. ‘It’s a win, win, win situation. The Government starts to get to grips with the NHS waiting list backlog right away, Rutherford could do with the income and NHS cancer patients get their treatment immediately.’
But some experts aren’t convinced that sharing the burden with the private sector is the solution, warning that not only do private clinics rely heavily on the same workforce as the NHS, but many of the treatments and specialities found in the NHS simply don’t exist in private hospitals.
And if things do go wrong, it is the NHS which has to pick up the pieces.
‘While private providers claim to be able to increase their capacity to treat NHS patients, it’s not clear how they expect to do this without drawing more of the medical workforce away from the NHS,’ says David Rowland, director of the think-tank the Centre for Health and the Public Interest.
Helen Buckingham, director of strategy at another think-tank, the Nuffield Trust, adds that private providers rely particularly on NHS surgeons and anaesthetists.
‘There’s no point in expanding private operations if it simply means the local NHS trust can’t find the staff to expand its own activity,’ she told Good Health.
There is also the question of whether private hospitals have the facilities, for instance, to treat an acute NHS caseload safely.
David Rowland points out: ‘For example, many private hospitals don’t have an intensive care unit, and if a patient has complications after surgery they may need to be transferred to an NHS hospital.’
The IHPN is adamant that there is more than enough staffing capacity in the private sector.
However, greater use of the private sector by the NHS highlights concerns about previous such deals during the pandemic, which critics say seemed to have benefited private hospitals far more than the NHS.
At the start of the pandemic, in March 2020, the Government bulk-bought private hospital services for a year while NHS hospitals were dealing with Covid.
Almost all the private hospital beds in England — 8,000 in total — were allocated for NHS use. The deal is estimated to have been worth £400 million a month, regardless of how many NHS patients were actually treated.
Private hospitals carried out 3.3 million NHS procedures during the year ending March 2021, according to a National Audit Office report, including about 100,000 inpatients. Yet this was only a fraction of the capacity the Government bulk bought.
A report last year by the Centre for Health and the Public Interest said the 26 private hospital companies delivered 43 per cent less NHS-funded healthcare under the contract than they did in the 12 months before the pandemic.
An investigation by the Health Service Journal found that two thirds of private sector capacity that was block-purchased by NHS England was left unused between June and September 2020.
Indeed, the IHPN analysis shows that pre-pandemic, in January 2020, private hospitals were carrying out almost 115,000 procedures a month on NHS patients, this dropped to fewer than 20,000 at the height of the pandemic in May 2020 — when the NHS had a bulk-buy contracts with the private sector.
The reasons for the poor use of private beds are complex.
During the pandemic, fewer patients came forward due to concerns about catching Covid in hospital, while strict hygiene measures meant that fewer patients could be seen than normal.
Private hospitals were also treating more patients with complex health problems such as cancer, rather than high volumes of hip replacements, for example.
Others claim confusion and poor communication over the contracts was to blame.
Last year, the number of NHS patients treated in the private sector remained down, despite a separate £10 billion deal between the NHS and the sector.
And yet the bulk-buy deals for beds between the NHS and the private sector were extended again in January 2022 for three months, until the end of March.
Behind all this are the lives of millions of NHS patients who are waiting for the care they need.
For Joseph Togher, a grandfather, the prompt surgery at the Spire Fylde Coast Hospital last September has been life-transforming. ‘If I’d had the operation at the NHS hospital, I would have had to wait nine months at least,’ he said.
He might still be waiting now, and yet thanks to the private hospital care, he’s enjoyed months without leg pain.
Appy days
Health apps that have an official stamp of approval. This week: Pillboxie, £1.79, AppStore on iPhones
Billed as the ‘easy way to remember your meds’, this app lets you record what tablets you need to take and at what time every day.
But what makes this reminder so user-friendly is it gives visual — rather than just text-based — prompts to take medicine. For example, if a drug has to be taken at 7am, a tablet will appear in an image of a pill box at that time and stay until the patient tells the app they have taken it.
Separately, the app can flash a list of ‘medicines due today’, which can be checked off by the patient as they go.
Source: Read Full Article