As obesity rates climb, so do the number of people receiving weight-loss surgery. One of the most frequently performed weight-loss procedures in the world—Roux-en-Y gastric bypass—is effective, but another procedure rarely performed in the U.S. is more effective at eliminating type 2 diabetes in patients with obesity. A new study from Washington University School of Medicine in St. Louis explains why.
Conventional wisdom has been that the less common procedure—called biliopancreatic diversion—has been better at reducing diabetes because it typically causes greater weight loss than the more common surgery. But in a small study, the researchers found that biliopancreatic diversion appears to be more effective at eliminating diabetes not just because of greater weight loss but because the procedure itself seems to make patients more sensitive to insulin.
Their findings are published online Oct. 3 in the journal Cell Metabolism.
“Our results help explain the high rate of diabetes remission in patients who have biliopancreatic diversion surgery,” said senior author Samuel Klein, MD, director of Washington University’s Center for Human Nutrition. “These data suggest that we should take a closer look to see whether it might be a better option for some bariatric surgery patients.”
The researchers compared the effects of the two surgeries on insulin and glucose sensitivity in patients who, after their operations, lost 20 percent of their body weight.
Insulin is the hormone that helps the body keep blood sugar under control. Being more sensitive to insulin allows cells in the body to use glucose in the blood more effectively and helps lower blood sugar.
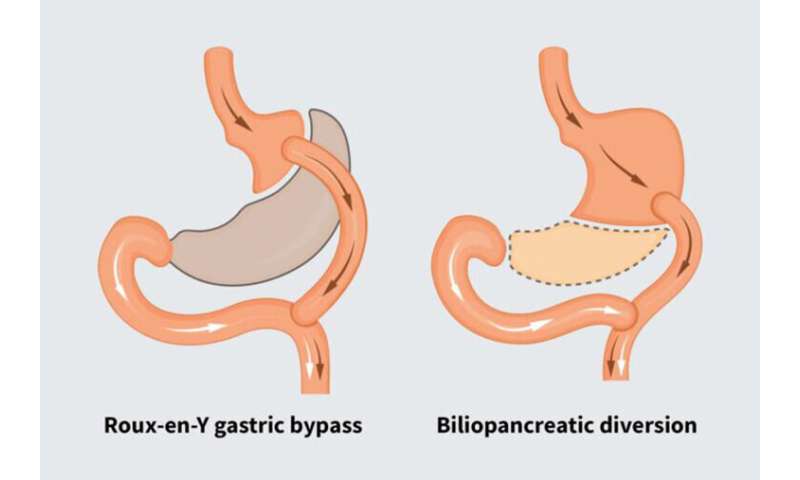
Roux-en-Y gastric bypass surgery makes a patient’s stomach smaller by sewing parts of the stomach together to create a pouch about the size of an egg. That pouch then is connected to the upper section of the small intestine, bypassing a small portion of the upper intestine.
Biliopancreatic diversion is a more complicated surgery. And past studies have found that patients who get the surgery tend to have more postoperative complications. In this procedure, the surgeon removes the lower part of the stomach, and connects the upper part of the stomach to the end of the small intestine, close to where it empties into the large intestine. Because so much of the intestine is bypassed, fewer nutrients from food are absorbed into the intestine, putting patients at a higher risk for long-term nutritional deficiencies. So patients must be closely monitored to ensure they’re getting adequate amounts of vitamins and minerals.
The less common procedure, however, results in better blood sugar control and higher rates of diabetes remission than Roux-en-Y gastric bypass surgery. Researchers didn’t understand why until, in this study, Klein’s team followed 24 patients, half of whom had Roux-en-Y gastric bypass surgery and the other half, biliopancreatic diversion.
The gastric bypass group in the study had average body mass indexes (BMI) of 48. A person’s BMI is calculated using weight and height. A higher BMI increases risk of health problems related to weight; a BMI of 30, for example, is considered obese. Those who had biliopancreatic diversion had average BMIs of 56.
The surgeries were performed at Catholic University in Rome. The operations were done overseas because biliopancreatic diversion is more commonly performed in Italy. In the U.S., some 228,000 bariatric surgical procedures were performed in 2017. Fewer than 3 percent were biliopancreatic diversion.
After surgery and a 20 percent loss of body weight, the study patients’ metabolic reactions to meals were measured, with close attention paid to their glucose levels, sensitivity to insulin and how much insulin they secreted after eating. The researchers found no difference in the benefit of surgery-induced weight loss to patients’ pancreatic function, in terms of insulin secretion, but patients who received biliopancreatic diversion surgery were found to be more sensitive to insulin.
Klein noted that while the patients had obesity, none had been diagnosed with type 2 diabetes. The study was structured that way because the researchers wanted to independently measure the insulin sensitivity after a meal, without potential complications caused by diabetes medications.
“This study demonstrates that biliopancreatic diversion has unique, beneficial effects on insulin action, independent of any weight loss,” he said.
As to whether that surgery should be preferred because of these findings, Klein said that’s less clear. The main consideration, he said, should be patient safety.
“This study demonstrates additional metabolic benefits from biliopancreatic diversion, compared to Roux-en-Y gastric bypass,” he said. “But the type of bariatric surgery performed on any individual patient depends on many considerations, including an assessment of the effectiveness and safety of the procedure, patient preference, and the surgeon’s experience.”
Source: Read Full Article