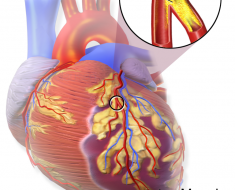
Blood pressure and cholesterol lowering drugs continue to improve survival in patients with hypertension after more than a decade, according to late breaking results from the ASCOT Legacy study presented today at ESC Congress 2018 and published in The Lancet.
Dr. Ajay K. Gupta, of the William Harvey Research Institute, Queen Mary University London, UK, said: “Patients in their mid-60s with high blood pressure were less likely to die from heart disease or stroke by age 75-80 if they had taken both calcium channel blocker-based blood pressure lowering treatment and a statin.”
The ASCOT Legacy study is the long-term follow-up of 8,580 patients from the UK who took part in the Anglo-Scandinavian Cardiac Outcomes Trial (ASCOT), which between 1998 and 2000 recruited patients with high blood pressure and three or more additional risk factors for cardiovascular disease.
Patients who took a newer blood pressure lowering treatment (based on a calcium channel blocker) for 5.5 years were 29% less likely to have died from a stroke ten years later than those taking an older regimen (based on a beta-blocker). There was a non-significant trend towards 10% fewer cardiovascular deaths with the newer therapy.
Patients with average (6.5 mmol/l) or below average blood cholesterol levels at the start of the trial who took a statin for 3.3-5.5 years were 15% less likely to have died from cardiovascular causes such as heart disease and stroke 16 years later than those randomised to placebo.
A subgroup of patients with above average cholesterol who received standard lipid-lowering therapy for 5.5 years had 21% fewer cardiovascular deaths over ten years of follow-up with the newer blood pressure therapy compared to the older one. There was a non-significant trend towards lower all-cause and stroke deaths with the newer treatment.
“These results are remarkable,” said Professor Peter Sever, of the National Heart and Lung Institute at Imperial College London, UK, who jointly led the study with Dr. Gupta. “We have previously shown that statins confer long-term survival benefits after trials have stopped, but this is the first time it has been found with a blood pressure treatment.”
Dr. Gupta said: “The findings provide further support for the use of an effective blood pressure lowering therapy plus a statin in most patients with high blood pressure.”
A main objective of the initial ASCOT trial was to find out whether a new treatment strategy for high blood pressure was more effective in preventing heart attacks than an old strategy. Patients with high blood pressure were randomly allocated to the new treatment of amlodipine (a calcium channel blocker) plus perindopril (an angiotensin-converting enzyme inhibitor) if needed to achieve the target blood pressure, or the old therapy of atenolol (a beta-blocker) plus bendroflumethiazide (a diuretic) and potassium if needed. The medicines were taken for a median of 5.5 years, when the trial was stopped because the newer treatment prevented more strokes and deaths. After the trial, patients went on to receive usual (or routine) care.
A second aim of the trial was to discover if a statin would provide added protection against coronary heart disease in patients with high blood pressure and cholesterol levels below 6.5 mmol/L. Patients with a blood cholesterol level of 6.5 mmol/l or less were randomly allocated to atorvastatin or placebo for 3.3 years, when the trial was prematurely stopped because atorvastatin prevented more heart attacks and strokes.3 Following this, patients were offered atorvastatin for the remainder of the blood pressuring lowering arm of the trial. During this 2.2 year period approximately two-thirds of patients previously assigned to either atorvastatin or placebo took atorvastatin.
A third aim of the trial was to evaluate the effectiveness of the newer versus older blood pressure lowering treatment in patients with high blood pressure and high cholesterol (above 6.5 mmol/l). These patients did not participate in the randomised lipid-lowering arm of the trial and all received standard lipid-lowering therapy for 5.5 years.
Source: Read Full Article