Choosing the correct individualised treatment for breast cancer depends upon determination of receptors for oestrogen, progesterone and HER2. The gold-standard method is currently immunohistochemistry (IHC). However, in 5 to 10 percent of cases, this testing of tumour tissue can produce false negative or false positive results – with serious consequences for the patient concerned. In a joint interdisciplinary project, researchers from MedUni Vienna have now demonstrated that diagnostic certainty can be significantly increased by a new investigation technique – namely by checking the gene expression of the receptors on a gene chip and then collating all the data in a mathematical model to derive an overall result.
Why are these findings so important? If one or more receptors that drive breast cancer is/are detected, then anti-hormonal therapy is the correct and most effective treatment. It inhibits the process and causes the receptors to flag. Comparatively stressful chemotherapy with its many side-effects is not necessary, although it could be used without any life-threatening consequences. However, if ICH shows that none of the receptors is present and that breast cancer has developed without their “drive”, then chemotherapy is usually used.
The problem arises when IHC has produced a “false positive” result due to a measurement error, that is to say if no receptors were actually present, despite the test results, so that hormone therapy was given. “In this case the error can be life-threatening,” says Wolfgang Schreiner from the Institute of Biosimulation and Bioinformatics.
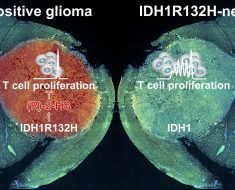
To increase certainty in determining receptor status, MedUni Vienna bioinformaticians looked at data from 3,241 patients from 36 clinical studies and developed a gene model for each receptor. Schreiner explains: “Before forming the protein material for the receptor, the gene first produces an RNA copy, a sort of ‘blueprint’ for the receptor. Using the gene chip, we can determine whether this RNA copy is present in the tumour tissue. That is an important marker.” At the same time, so-called co-genes were identified in each case, these being the second-commonest genes associated with receptor formation.
The information from IHC and from expression of the receptor genes and the co-genes was fed into a robust mathematical model, which serves to eliminate false results fairly accurately. “One could continue this series indefinitely,” says Schreiner. “We could now feed additional omics data sources into our analysis, one after the other – until we have reduced false positive or false negative results to virtually zero. We will then have certainty.”
In future, this fusion of omics data, that is molecular biological data seen from various angles, will allow scientists to keep increasing precision in diagnosis and treatment – in keeping with the spirit of personalised medicine. “Our task lies in utilising advanced mathematics for the benefit of precision medicine,” says Schreiner.
Use in clinical practice
“The challenge is to offer tailor-made therapy so that we can give the correct treatment in a more targeted and accurate way, thereby avoiding the use of unnecessary treatments and the associated side-effects. The overall aim of the Comprehensive Cancer Center of MedUni Vienna and Vienna General Hospital (CCC) is to treat patients more selectively and individually,” says Heinz Kölbl, head of the Division of General Gynecology and Gynecologic Oncology, which also participated in the study.
Source: Read Full Article