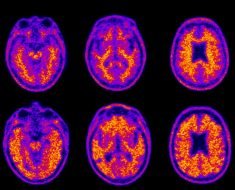
Healthcare providers and researchers rely on screening questions to detect patients who may be at risk for developing Alzheimer’s disease and other aging-related problems, but how these questions are worded may be confusing or trigger emotional responses. According to Penn State researchers, this may result in patients who answer the same questions differently, and for different reasons.
In a study with older Pennsylvania adults, researchers asked participants a variety of common screening questions and then followed up to learn more about how each participant felt about those questions.
For example, when asked “Have you had problems with your memory recently?” one patient may interpret “recently” as within the same week while another may interpret it as within the month. Or, a third may be frightened by trouble with their memory and brush off the question altogether.
Nikki Hill, assistant professor of nursing at Penn State, said the results will help clinicians and researchers ask better questions and better interpret patient responses.
“If someone has concerns about their memory, that could be important for a lot of different reasons,” Hill said. “It could mean they have a problem that may continue to get worse, or maybe it’s impacting them emotionally, or maybe they just need more information. So we’re trying to learn the best questions to ask to really get at what our patients are experiencing and how best to respond.”
According to previous research, older adults who report memory problems but score in the normal range on cognitive tests are up to twice as likely to develop Alzheimer’s later.
Jacqueline Mogle, assistant professor at Penn State, said creating good questions is important not only for screening patients early for the disease, but also so researchers can ask good questions when studying these populations.
“When we ask people questions, we assume that they see the questions the same way we do,” Mogle said. “However, that clearly isn’t the case. What we might see as a straightforward question—like ‘Do you have problems with your memory?’—may mean something very different for older adults. Right now it isn’t clear how they are deciding to answer the question.”
The researchers recruited 49 older adults in central Pennsylvania who did not have dementia to participate in the study. Each participant was asked a variety of questions commonly used to screen for Alzheimer’s disease. After the participant answered, the researchers asked them follow-up questions about how and why they answered the way they did to help identify possible problems with the screening questions.
After analyzing the data, the researchers found 13 different types of problems in the screening questions. The two most common problems were vagueness—”There are multiple ways to interpret the question”—and an assumption that their behavior or experience is always the same. For example, they sometimes may have trouble remembering the day of the week but not always.
The researchers also found that some questions tended to provoke an emotional response. For example, one question asked the participant to “rate” themselves or their memory compared to others, which some participants associated with dips in confidence and feeling poorly about themselves.
Hill said that learning to ask better questions about a person’s memory could help improve clinicians’ understanding of their patients’ unique experiences.
“For older adults, problems with memory and thinking is something that’s experienced very differently from person to person,” Hill said. “However, in the research to date, we don’t tend to reflect how complicated of an experience that is. If we really want to understand how people are experiencing early symptoms and what is influencing their reporting of symptoms, we need to get at more of that individual experience, and our questions that we currently use aren’t capturing it.”
Hill added that it would be helpful for future studies to examine the best ways to reword and standardize screening questions to help reduce cognitive biases.
Source: Read Full Article