By studying a rare liver disease called Alagille syndrome, scientists from Cincinnati Children’s and the University of California San Francisco (UCSF) have discovered the mechanism behind an unusual form of tissue regeneration that may someday reduce the need for expensive and difficult-to-obtain organ transplants.
The team’s findings, published in the journal Nature, show that when disease or injury causes a shortage in one critical type of liver cell, the organ can instruct another type of liver cell to change identities to provide replacement supplies.
This discovery was made in mice but in years to come may lead to a viable treatment for human disease. If ongoing follow-up studies succeed, the medical world may gain an alternative method for repairing tissue damage that does not require manipulating stem cells to grow organs from scratch in a lab dish.
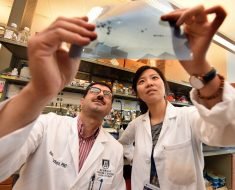
“We have known for a long time that the liver has more ability to regenerate than other organs. Only recently have we had the tools to study this ability in depth. Now we have a high-level understanding,” says Stacey Huppert, PhD, a developmental biologist in the Division of Gastroenterology, Hepatology and Nutrition at Cincinnati Children’s, and one of two leading co-authors of the paper.
“Our study shows that the form and function of hepatocytes—the cell type that provides most of the liver’s functions—are remarkably flexible. This flexibility provides an opportunity for therapy for a large group of liver diseases,” says Holger Willenbring, MD, PhD, the study’s other senior co-author and a member of the Department of Surgery, the Eli and Edythe Broad Center of Regeneration Medicine and Stem Cell Research, and the Liver Center at UCSF.
What is Alagille syndrome?
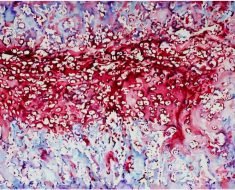
Alagille syndrome (ALGS) is a rare, inherited genetic disorder due to deficiencies in the Notch pathway, which plays an important role in cell development. ALGS is best known for disrupting the liver’s plumbing system, which consists of tubes called bile ducts that deliver bile made in the liver to the intestine. The disorder occurs in about 1 in 30,000 people, and in most cases, the problems caused by the condition emerge during infancy or early childhood.
The extent of the condition can range from having too few or too narrow bile ducts to missing all bile ducts in the liver. As a result, the bile that normally helps the body digest fat and carry away toxins backs up inside the liver where it causes severe damage. In many patients with ALGS, bile duct function can be managed and sustained. However, up to 50 percent of patients eventually need a liver transplant, often during childhood.
A Quicker Method of Self-Repair
Every day, the liver takes a beating as it processes everything from medications to alcohol consumption. All these “insults” have prompted the liver to develop a rapid healing ability that does not rely on stem cells, the co-authors say.
“In addition to making more of themselves, liver cells can switch their identity to produce a liver cell type that is lost or, in the case of severe ALGS, never formed,” Willenbring says.
“Previous research has detected adaptive reprogramming in other organs, but it typically involves only a few cells at a time. Our study shows that cells switch their identity at a massive rate in the liver,” Huppert says.
Discovering this phenomenon and learning how it works took nearly five years. The team included co-first authors Johanna Schaub and Simone Kurial from UCSF and Kari Huppert from Cincinnati Children’s.
The researchers generated mice that lack cholangiocytes, the type of liver cell that forms bile ducts. Like patients with severe ALGS, these mice quickly developed signs of liver injury. However, over time the mice’s symptoms improved because hepatocytes converted into cholangiocytes and formed fully functional bile ducts.
In July 2017, another study published in Nature reported that cholangiocytes can become hepatocytes if their ability to regenerate is impaired. Viewed together, the two studies suggest that switching of cell identity is the main backup mechanism for liver repair.
The new study further shows that the Notch pathway, which is essential for forming bile ducts but defective in patients with ALGS, can be replaced by another pathway. This process is regulated in the injured liver by transforming growth factor beta (TGFβ), a protein that controls cell growth. This discovery is a vital step in identifying targets for therapies that might control this process.
Next Steps
Now the research team is working to determine the precise set of proteins, called transcription factors, that work together to carry out the identity-switching process.
“Using transcription factors to make bile ducts from hepatocytes has potential as a safe and effective therapy,” Willenbring says. “With our finding that an entire biliary system can be ‘retrofitted’ in the mouse liver, I am encouraged that this eventually will work in patients.”
Source: Read Full Article