The commensal bacteria in the human gut helps to maintain homeostasis and contribute to the health of their host. These microorganisms exist in a careful balance and, if disrupted, this can contribute to the development of disease.
Changes to the microbial composition of the gut can increase susceptibility to infections and has been linked to various inflammatory diseases and cancers, including colorectal. Environmental factors known to influence the development of cancer, such as diet, lifestyle, and medication, are also associated with changes to the microbiota. Therefore, the effects of microbial dysbiosis on the development of cancer is an interesting area of research. Studies indicate a link between colorectal cancer and gut microbial composition, with several influential bacterial species identified.
Microbiota and Gut Health
A diverse and balanced microbiota is thought to be important for a well-functioning immune system. The gut hosts 70% of the body’s resident microbes, containing around 100 trillion microorganisms (including bacteria, viruses, and fungi) made up of approximately 1000 (mainly bacterial) species. Although the composition of gut microbiota varies between individuals, there are three prevailing phyla: firmicutes (make up 30%-50%), bacteroidetes (20%-40%), and actinobacteria (1%-10%).
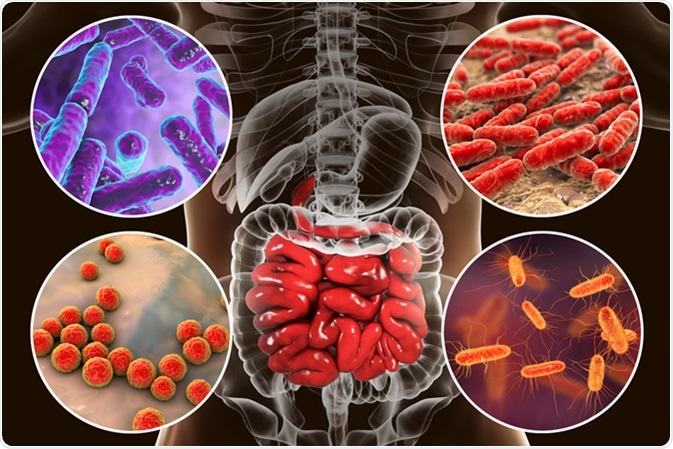
Studies in germ-free mice indicate that, collectively, gut microorganisms contribute to the health of their host in a variety of roles, including:
- Physiological – by promoting vascularity, and the activity of digestive enzymes, increasing the thickness of muscle cell walls, production of cytokines, and function of the mucosal barrier
- Immunological – by promoting the production of serum immunoglobulins, intraepithelial lymphocytes, humoral components and T-cell cytokines, maintaining the size of Peyer’s patches and modifying T-cell repertories
- Metabolic – by participating in anaerobic carbohydrate and proteolytic fermentation which can affect gene expression, the differentiation and proliferation of epithelial cells in the intestine, vitamin and mucus production, and ion absorption. These metabolic activities increase the generation and storage of energy from dietary intake, regulate fat storage, and are involved in the growth of bacteria. Some of the resulting metabolites can be toxic to the host
- Structural – by helping with the regeneration of epithelial cells, maintenance of intestinal villi and crypts, and the process of angiogenesis
- Protective – by inhibiting infection of the gut by invading pathogens through resistance or interference mechanisms
Therefore, understanding the variety of effects that gut dysbiosis has on host response and inflammation is important for understanding the role of the microbiome in cancer.
The Potential Impact of Microbiota in Colorectal Cancer
The cause of colorectal cancer is generally considered to be environmental, rather than genetic. An increasing incidence in all western, and many developing, countries, indicates that the western lifestyle may be a major contributor to disease development. Colorectal tumors are made up of cancerous and non-cancerous cells, and many microorganisms. The involvement of microbiota in colorectal carcinogenesis is becoming increasingly evident.
Microbes are thought to be involved in up to 20% of cancers, particularly with some gastrointestinal and liver carcinomas. Unlike gastric cancer, which is strongly linked to a single bacterial species (Helicobacter pylori), CRC development appears to be influenced by the composition of the microbial community, rather than a single pathogen.
Lending support to this notion is the fact that the incidence of colon cancers is around 12-fold greater than those in the colon than the small intestine, where the levels of bacteria are more than one million-fold higher. CRC was first linked to gut microbiota in 1975, when conventional rats were shown to be more prone to the development of colorectal tumors than germ-free rats. These results have since been replicated.
Evidence suggests that the composition of the gut microbiome differs between patients with colorectal cancer and healthy individuals. Modification of inflammatory processes within the host colonic mucosa by residing microorgansims may be able to influence either the development or prevention of CRC.
The following differing hypotheses have been proposed to explain how microbial dysbiosis contributes to the development of CRC:
Alpha-bug theory: a primary pathogen species (such as enterotoxigenic Bacteroides fragilis, ETBF) is able to remodel the microbiome to activate a pro-carcinogenic environment: promoting the transformation of epithelial cells and inflammatory responses, possibly by the release of IL-17 and TH17
Driver-passenger theory: intestinal bacteria, termed “bacteria drivers”, (such as ETBF), induce epithelial DNA damage, aggravate inflammation, and produce genotoxins that lead to cell proliferation and mutations, and, eventually, to tumorigenesis. This environment allows other “passenger” bacteria to thrive (such as Fusobacterium spp) which encourages tumor progression. As the tumor progresses, constant inflammation damages the intestinal barrier, giving bacteria an entry to the tumor tissue. The bacteria and their metabolites continue to stimulate tumor growth, e.g. through the release of metabolites or activation of IL-17 cytokines.
It is likely that aspects of both of these processes contribute to the development of CRC.
Evidence
Mouse models of altered immune and inflammatory responses indicate that microbial dysbiosis is enough to promote the development of cancer, as shown by:
- Transferring the microbiota from mice with tumors induces tumor development in healthy animals
- Tumor development is prevented when mice with a genetic predisposition to develop CRC are treated with antibiotics
In addition, retrospective human cohort studies are investigating the microbiome of healthy individuals vs. patients with CRC or adenomatous polyps, or differences in the intestinal microclimates between healthy and tumor tissue of patients.
Several studies have shown colonic dysbiosis from patients with CRC by sequencing the 16s bacterial rRNA from digestive tissues or feces. Although, as yet, no defining causal species have been identified in the development of CRC, some common bacterial species have emerged. In particular, Streptococcus bovis, H. pylori, Bacteroides fragilis, Enterococcus faecalis, Clostridium septicum, Fusobacterium spp. and Escherichia coli.
These studies endeavour to define a CRC-associated microbiome. The diversity that exists within the gut microbiota supports the idea that dysbiosis could lead to a pro-carcinogenic environment. However, the exact mechanisms by which changes in microbial composition occur are not well elucidated, and it is not understood whether dysbiosis is a cause or a consequence of CRC.
Conclusion
Evidence is growing to indicate that the gut microbiota has a large role in the development of CRC. Several mechanisms may be involved, including disruption to inflammatory and metabolic processes and the production of genotoxins. Further understanding of the mechanisms involved will facilitate the development of methods with which to target the microbiota for the control and prevention of CRC, e.g. probiotics or fecal transplantation. Greater knowledge on the interactions between potential causative microorganisms and the host environment will require functional studies using metabolomics and RNA sequencing technologies.
Sources
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3625019/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4180221/
- www.ncbi.nlm.nih.gov/pmc/articles/PMC4716055/pdf/WJG-22-501.pdf
- https://www.nature.com/articles/srep26337
Further Reading
- All Colorectal Cancer Content
- What Causes Colorectal Cancer?
- What is Colorectal Cancer
- Colorectal Cancer Diagnosis
- Colorectal Cancer Prevention
Last Updated: Oct 11, 2018
Written by
Rebecca Woolley
Rebecca has spent her working life in medical communications. With a career that has spanned three continents, she has a breadth of experience in a variety of roles covering numerous therapeutic areas. She enjoys the variety that writing brings, with areas of research including type 2 diabetes, anticoagulation therapy, and chronic obstructive pulmonary disease.
Source: Read Full Article