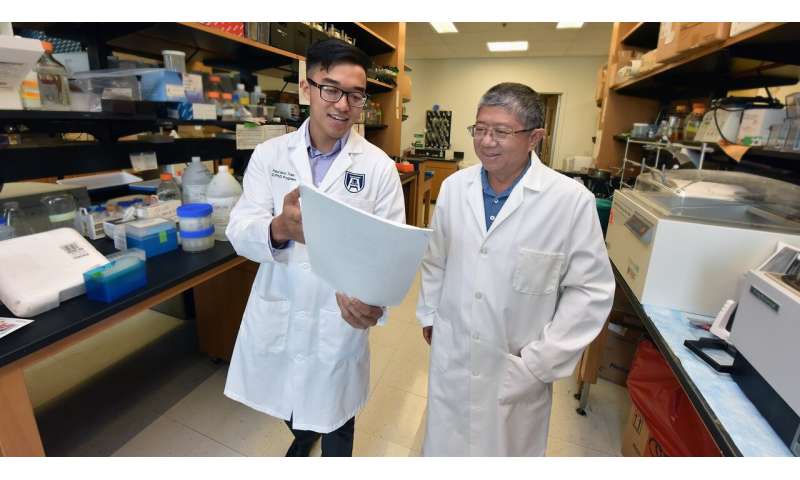
Paul Tran is working to develop a highly predictive genetic risk score that will tell parents whether their baby is at significant risk for type 1 diabetes.
The ultimate goal, says the MD/Ph.D. student at the Medical College of Georgia at Augusta University, is to prevent a condition that typically surfaces in youth, destroys the pancreas, and leads to a lifetime of insulin therapy or a pancreas transplant.
Tran is now putting together thousands of gene variants associated or already considered causative for type 1 diabetes found in thousands of individuals worldwide over nearly two decades. He’ll be using an algorithm that works similar to our brains, called a feedforward neural network, to turn that massive data into an individual child’s genetic risk score.
He hopes to tell parents with at least 50 percent probability—five times better than the current scoring system—that their child will develop type 1 so the child can be enrolled in a program to prevent the condition that results from a collision of genetics and environmental factors from infections to early food exposures.
In a bit of a full circle, Tran says a more accurate score should in turn improve prevention trials by better ensuring more appropriate study enrollees so outcomes are super relevant, all the while identifying still more causative gene variants and more treatment targets.
“Our goal by the end of this project is to develop a test that can be used for newborns,” says Tran, who recently received a three-year research fellowship award from the National Institute of Diabetes and Digestive and Kidney Diseases to pursue that goal.
“We want to stop it before it starts or at least at the very beginning,” says Dr. Jin-Xiong She, Tran’s mentor, director of the MCG Center for Biotechnology and Genomic Medicine and Georgia Research Alliance Eminent Scholar in Genomic Medicine.
She’s also principal investigator for prospective studies in Georgia and Florida called TEDDY—The Environmental Determinants of Diabetes in the Young—an international initiative also funded by the NIDDK following nearly 9,000 children and their families considered at risk for type 1 because they were found to have two genes already considered highly causative. Since TEDDY started, the children have been closely followed through puberty as scientists try to determine how genetics—which accounts for maybe 60 percent of risk, She says—and environment contribute to the autoimmune disease. Peak ages for type 1 diabetes to surface are 2-4 and 12-15.
It’s the extensive data collected by TEDDY as well as data from the also international, now completed Type 1 Diabetes Genetics Consortium, comparing the genes of individuals with and without type 1 diabetes to identify more causative genes, that is included in the extensive genetic pool for Tran’s project.
He’ll use data he finds in the samples from the Type 1 Diabetes Genetics Consortium from people who have type 1 diabetes to train his genetic prediction model and TEDDY samples, a mix of young people who have and have not developed disease but are already considered at risk, to refine his model’s ability to be highly predictive.
“We really want to use as many as possible,” says Tran, so he’s being as inclusive as possible with associated gene variants from thousands of individuals being placed on an immunochip from two of the largest type 1 diabetes studies ever.
Using high throughput technology, Tran will analyze patients’ genetic information to see how the large number of variants might work together to cause type 1 diabetes. To calculate an individual child’s risk, they will use the feedforward neural network, an algorithm inspired by how neurons act and interact to help us assemble and process complex thoughts.
“In this case we are trying to predict who will develop type 1 diabetes based on their genetics,” says Tran.
“We are trying to use technology developed by groups like Google and apply them to biomedical questions and type 1 diabetes, specifically,” adds She, referencing using the neural network, a form of artificial intelligence, to help digest and interpret large, complex data so it is useful.
Tran’s current steps include optimizing the data included on the chip. New data on genes associated with type 1 also continues to be published, which means the data will continue to expand, She adds.
Tran’s preliminary studies that enabled his NIDDK research fellowship used just the TEDDY information, and Tran saw that the feedforward neural network is more predictive than other problem-solving approaches and that just going from analyzing 42 to 112 gene variants enabled much better prediction of type 1 diabetes in a child’s future. Now he is looking at many thousands.
“We should be able to build a better model,” Tran says. “Using all the genes available today we can better identify a larger group of children who will end up developing diabetes.”
“Being able to identify the true high-risk population much, much better than we can do in TEDDY is a critical thing that has to be done,” says She. “Our best prediction is about 10 percent risk now.”
To further enhance accuracy, Tran wants to eventually add significant environmental factors—like those being identified by TEDDY—but will start with this most comprehensive genetic profile to date.
Genetic risk scoring systems already are being marketed for problems like often lifestyle related type 2 diabetes and cardiovascular disease. Others are looking at genes associated with staying well as you age in individuals termed the wellderly.
“I think a lot of diseases will end up having genetic risk scores that everyone can look at and try to take the temperature on your risk in the future,” Tran says. The ideas and models he is developing now definitely are applicable to other diseases, he notes, if you have good data.
Type 1 diabetes affects about 1.25 million Americans, according to the American Diabetes Association. The autoimmune disease typically surfaces in youth and destroys the insulin-producing beta cells in the pancreas. Type 1 complications are similar to type 2 complications and include heart and blood vessel disease as well as nerve, kidney, eye and foot damage.
Source: Read Full Article