Heart disease, stroke, sepsis, and cancer collectively cause the greatest number of deaths worldwide. They also have something else in common: all of them are associated with activated platelets, the cells that circulate in our bloodstreams and normally help form blood clots to stop bleeding and promote healing when we are injured, but can also contribute to dangerous blood clots, tumors, and other problems. Several antiplatelet drugs have been developed to combat platelet-related conditions, but their effects are not easily reversible, and patients taking these drugs are at risk of uncontrolled bleeding if injured. Also, if these patients need to undergo surgery, they must stop their treatment for up to a week prior to the procedure, which raises their risk of developing blood clots.
Now, a team of researchers at the Wyss Institute at Harvard University and several collaborating institutions has created a drug-free, reversible antiplatelet therapy that employs deactivated “decoy” platelets that could reduce the risk of blood clots and potentially prevent cancer metastasis as well. The research is reported in Science Translational Medicine.
“The reversibility and immediate onset of action are major advantages of our platelet decoys, and we envision them to be useful in hospital-based situations such as preventing clotting in high-risk patients just before they undergo surgery, or when given alongside chemotherapy to prevent existing tumors from spreading,” said first author Anne-Laure Papa, Ph.D., who was a postdoctoral fellow at the Wyss Institute working with the Institute’s Founding Director, Donald Ingber, M.D., Ph.D. when the research was carried out and is now an Assistant Professor at George Washington University. Ingber is also the Judah Folkman Professor of Vascular Biology at Harvard Medical School and the Vascular Biology Program at Boston Children’s Hospital, as well as Professor of Bioengineering at Harvard’s School of Engineering and Applied Sciences.
Canceling clots
The decoys are human platelets whose outer lipid membrane and innards have been removed in the lab via centrifugation and treatment with a detergent. Because they are essentially empty, the decoys are about one-third the size of normal platelets, but they retain the majority of the adhesive proteins on their surfaces. The decoys can still use these surface molecules to bind to other cells that naturally occur in the bloodstream, but they are unable to activate the clotting process.

When the decoys were perfused into a microfluidic, blood-vessel-mimicking channel and exposed to platelet-stimulating chemicals, they did not display normal clotting behavior. And, when the researchers added decoys to normal human blood (one decoy for every five platelets) in the channel, they found that the normal platelets’ ability to aggregate and bind to the channel’s walls was reduced.
“The decoys, unlike normal intact platelets, are unable to bind to the vessel wall and likely hinder the normal platelets’ ability to bind as well. A way to imagine this would be that the decoys are fast-moving skaters skating along the wall of an ice rink, and their high speed prevents other skaters from getting to the wall, thus limiting them from slowing down and grabbing onto it.” Papa explained.
Importantly, the scientists were able to rapidly reverse the decoys’ inhibition of normal platelet activity simply by adding fresh platelets to the channels. Administering platelets to patients intravenously is already a common procedure in hospitals, so a patient with decoy platelets who needed to quickly regain the ability to form blood clots because of an injury or surgery could be easily treated within a short time frame. The decoys also could be created from platelets removed from the same patient, thus offering a form of personalized cellular therapy that would not trigger an immune reaction.
The researchers then tested their decoys in rabbits and found that the same 1:5 ratio of decoys to normal platelets in their blood prevented them from developing blood clots after a blood vessel injury. Rabbits and humans have similar blood platelet counts and platelet sizes, so it is likely that they would have the same effect in human patients.

Thwarting tumors
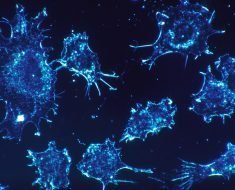
In addition to binding to each other and blood vessel walls, platelets are known to bind to cancer cells, protecting them from the body’s immune system and thereby helping them form new metastatic tumors at distant sites. When the team perfused normal platelets and human breast cancer cells into their microfluidic channels, the cancer cells stuck to and started invading the walls of the channel, similar to their behavior in forming new tumors. Encouragingly, adding decoys along with normal platelets almost completely prevented the platelets from helping the cancer cells invade the channel wall, suggesting that they could prevent the formation of new tumors.
To confirm this potential, the researchers injected mice with either human platelets or a combination of platelets and decoys, and then with human breast cancer cells. The team found that the mice that received the platelets plus decoys developed significantly smaller and fewer metastatic tumors than the ones that received normal platelets. While they have not yet been tested in humans, it is possible that one day these decoys could be infused into patients during chemotherapy to prevent existing tumors from spreading, or injected during cancer surgeries to stop released tumor cells from forming new tumors elsewhere in the body.
Papa’s lab is continuing to work on this technology to ensure that the decoys can last longer in the bloodstream for enhanced effectiveness, and studying whether they can be loaded with drugs to help deliver therapies directly to the sites of blood clots and tumors, or possibly even kill circulating tumor cells in the bloodstream.
Source: Read Full Article