LaTasha Unseld was nervous, but she wanted to read the 5,283 words she’d written. And she would not let her headache stop her. After all, as she told the court, her headache was due to her ex.
Doctors told Unseld she was one punch away from severe brain trauma after her ex-partner, Demetrius Singleton, choked and beat her in 2014. Singleton, the father of her children and her partner for two decades, is in prison for aggravated domestic battery, strangulation and sexual assault.
Recent research on head trauma has mainly focused on NFL athletes, whose brains have been shown to be damaged after years of hits to the head, and injured veterans.
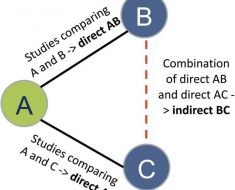
But survivors of domestic violence often experience blows to the head, as well. Chicago researchers hope to build on the research on football players in a way that can help survivors of domestic abuse.
“Everything we hear in the media is more focused on men,” said Dorothy Kozlowski. “But, in reality, women get traumatic brain injuries just as much as men do.”
Kozlowski, a professor of biology and director of the neuroscience program at DePaul University, recently received a grant from the school’s University Research Council to study repeat concussions. She hopes to find out if people hit in the head multiple times, especially women in abusive relationships, might be more susceptible to diseases like chronic traumatic encephalopathy (CTE) or Alzheimer’s.
“They got hit to the head by a fist, by a chair, by whatever it was, by being thrown against the wall,” said Kozlowski. “Any kind of hit to the head that they would receive is similar to what someone on a football field could receive.”
She estimates that anywhere between 60 and 90 percent of domestic violence victims have experienced at least one head injury. Injuries are often to the brain, skull or face. It’s also possible to experience multiple injuries to the head and neck within one violent episode.
That’s what happened to Unseld.
“I was never afraid of him until that terrifying night,” she said in her victim impact statement. “That night he was a stranger in my home.”
Singleton beat her so badly, she said, she doesn’t know how she escaped. She was bruised from “head to toe” and spent days in the hospital for a head injury and trauma, according to her medical records.
A 2016 study estimated that 23 million women in the United States could be living with a brain injury from interpersonal violence.
Dr. Darryl Kaelin, medical director of the Frazier Rehab Institute in Louisville, Ky., has worked in brain injury rehabilitation for decades and has seen a range of injuries. He recalled a client whose boyfriend hit her in the head with a sledgehammer that left her with cognitive deficits and dependent on her mother at age 30.
Despite the severity of the injury, Kaelin said, “when you’ve had a change in your mental status or a change in the way your brain functions, even for a temporary amount of time, that is an injury to your brain.”
Ember Urbach, who leads training sessions for the Chicago Metropolitan Battered Women’s Network, understands the experience of a brain injury. She has had three, most recently in 2011, after banging her head against her husband’s while loading the dishwasher. That accident, while in a healthy relationship, has had huge consequences, she said. She now has migraines and memory loss.
“Very simple tasks became very difficult,” she said. She had trouble reading because she couldn’t focus on the words.
“The whole thing made me feel insane,” Urbach said. She quit both of her jobs—substituting at a preschool and categorizing photographs—because she could not concentrate. People thought she was depressed or tired, she said.
Researchers of brain injury and domestic violence say symptoms of brain injury can make it more difficult for a woman to care for herself or her children, which can make her less likely to leave her abuser.
In December, Kozlowksi hopes to take a team of Chicago researchers and domestic violence advocates to Phoenix to learn how to better assess survivors of brain injuries from Jonathan Lifshitz, director of the University of Arizona’s College of Medicine’s Translational Neurotrauma Research Program.
Lifshitz, who spoke at a recent DePaul conference on domestic violence and brain injury said CTE can only be diagnosed after death, and no domestic violence survivors’ brains have been studied in the same way football players’ brains have. He said researchers are just beginning to understand what’s even possible to know.
Kathy Doherty, Chicago Metropolitan Battered Women’s Network executive director, said the nonprofit plans to add questions within its intake process to ascertain possible brain injuries, such as asking about headaches and memory loss.
Unseld, a woman who used to pride herself on remembering a slew of appointments on any given day, now has to rely on phone reminders. She said she forgets what her daughter tells her minutes later.
“I know it has to be something with the concussion,” she said, showing the color coded system on her phone calendar she uses to keep things straight. “I never had to do this before.”
She hopes that speaking out will help other women have the strength to recognize when they are in danger and to leave abusive relationships.
Source: Read Full Article