The finger prick from a thorn generates an immediate sensory response. In that instant, neurons at the injury site fire an electrical signal along a nerve fiber to the central nervous system. Our brain notes to avoid further encounters with thorns and the painful insult subsides.
But some health conditions cause pain that is chronic, debilitating, and often confounding. The pain may originate in organs deep inside the body and may affect their function. A long course of medicine to treat the discomfort could have undesirable side effects, including drug dependency.
Interstitial cystitis/bladder pain syndrome is a condition that affects millions in the United States alone. Those affected experience abdominal discomfort that increases as their bladder fills, which in turn causes excessive urinary urgency and frequency. Within the past decade, neuroscientists studying this syndrome and other neurologic conditions have turned to a biological technique called optogenetics, which uses gene therapy and light to turn neurons on and off, and potentially to turn chronic pain signals off.
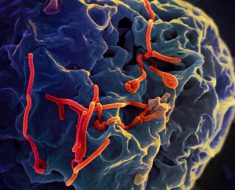
To achieve an optogenetic effect, researchers can induce expression of light-sensitive proteins, called opsins, in neurons that sense pain. Opsins can be derived from algae or other organisms, but also are part of the eye’s machinery that senses light. Because they can be tuned to specific wavelengths of light, they have a promising role to play in treating a variety of conditions that involve excitable cells that produce electrochemically charged impulses, such as neurons and muscle fibers. In pain-sensing neurons, opsins can be used to activate or deactivate pain signals coming from the peripheral nervous system.
In a study published in the Nov. 22, 2017, issue of Scientific Reports, researchers with funding from the National Institute of Biomedical Imaging and Bioengineering (NIBIB) reported the first use of optogenetics to reduce bladder pain. Their results in mice offer hope for much needed human therapy.
“This study represents a complex new technology with enormous potential to understand how the peripheral nervous system interacts with the bladder, leading to new therapies to manage bladder function and pain,” said Michael Wolfson, Ph.D., Director of the NIBIB program in implantable and assistive medical devices.
In their study, teams from Washington University School of Medicine in St. Louis and the University of Illinois at Urbana-Champaign performed tests with mice bred with light-sensitive opsin proteins expressed in pain-sensing neurons. They also implanted some mice with small, flexible, light-emitting diode (LED) devices that are wirelessly controlled. By flipping the on-switch of the LED, they activated the opsin, which silenced the neuronal signal, resulting in pain relief for the animals. In a previous study, they showed that the approach could control pain in the extremities of mice; in the present study, the researchers tested whether a similar optogenetic system could be used to control neurons deep inside the body, with mice affected by bladder pain.
Co-senior author Robert W. Gereau IV, Ph.D., is the Dr. Seymour and Rose T. Brown Professor of Anesthesiology and director of the Washington University Pain Center. His team studies the cellular and molecular mechanisms of chronic pain and collaborates with clinicians whose patients are affected by the disorder. “Urologists are used to dealing with problems that originate in the bladder, and one prevailing hypotheses is that this problem is largely a dysfunction of the nervous system,” he said. “This optogenetic approach could be a drug-free way to do a local nerve block coming from the bladder.”
Co-senior author John A. Rogers, Ph.D., professor of materials science and engineering at the University of Illinois, designed the implanted LED devices used in the study. His team builds miniaturized, wirelessly powered implantable devices that are flexible and stretchable, so they do not impede the animals’ movement. They previously had developed devices implanted in the cranium of mice that interfaced directly with the laboratory animals’ brains.
“We were able to develop fully implantable devices for wireless control and delivery of light to targeted, soft-tissue regions of the animals, which was the bladder in this case,” Rogers said. “These systems are unique in their ultrathin, flexible designs; their battery-free operation; and their use of microscale light emitting diodes, thereby enabling stable operation in the animal, without any measurable adverse effects over many months.”
The researchers performed a set of tests using mice whose genome had been modified to express an opsin that is responsive to green light. They designed an experiment to use these wireless LED devices to activate the opsin, leading to silencing of the pain-sensing neuron, but only in the selected area of the bladder.
The researchers performed three tests in mice. In the first, they recorded electronic signals of abdominal-muscle response during a procedure to fill the bladder. Both normal mice and mice bred with the light-sensitive opsin gene were included in the test. When LED light from a fiber-optic cable illuminated the bladder, the electronic signal measurements showed that genetically modified mice received pain relief during light exposure.
The researchers next performed a test to measure referred pain, in which the pain is felt at a location different from the original site of the stimulus. In this case, the pain from the bladder is felt in the abdomen wall. “Patients that have bladder pain syndrome are hypersensitive to pressure on the abdomen,” Gereau said. “You can measure hypersensitivity quantitively using mechanical pressure on the abdomen.” In this test, animals with the opsin protein received total reversal of referred pain.
They designed a further test to determine whether mice with bladder pain would respond to pain relief from the activation of a wireless LED implant. The researchers placed mice in a v-shaped maze, where the animals could move freely from one end to the other, while a camera recorded their movements. Mice without bladder pain—whether they were bred with a light-sensitive opsin or not—predictably preferred to huddle either distant corner of the maze, with no preference for the side of the maze where the LED was turned on. “Mice like to hide in the corners of these things,” Gereau explained.
The team observed much different results for another set of mice experiencing bladder pain. Those without a light-sensitive opsin protein found a random corner to huddle. But those with the light-sensitive opsin protein and an implanted LED preferred the end of the maze at which researchers wirelessly activated the LED.
“The mice are in this maze for 20 minutes and they vote with their feet where they want to be,” Gereau said. “To my knowledge, it is the first time any of us in the pain field have been able to convincingly demonstrate that an animal has ongoing pain that we are able to relieve in a moment-by-moment basis.”
For the approach to eventually be applied to human chronic pain, significant challenges in gene therapy would need to be overcome, but the hardware could be ready very soon. “We use implantable stimulators already—we have spinal cord stimulators, peripheral nerve stimulators, and deep-brain stimulators—all these things are used to treat neurologic conditions,” Gereau said. “We’re trying to come up with safe, non-addictive ways to treat pain.” He envisions that patients could use a smart-phone app to adjust activation of implanted LEDs to regulate their chronic pain.
Source: Read Full Article